Providers, their organizations, and the market in general are greatly anticipating CMS’ mandated publication of the MACRA final rule by November 1, 2016.
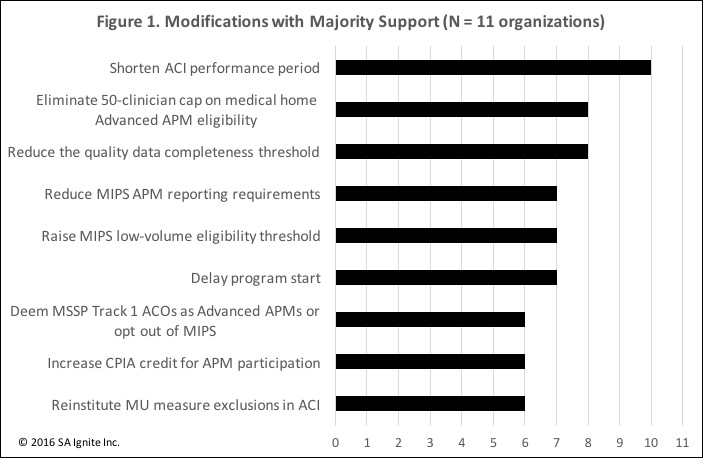
To get a broader understanding of the public response to the MACRA draft rule, we classified and counted the comments submitted from 11 leading organizations, collectively representing the majority of Medicare providers and their organizations: AAFP, ACP, AHA, AMA, AMDIS, AMGA, AMIA, CHIME, HFMA, HIMSS, and MGMA. This is only one of many possible approaches to measuring comment “popularity”, but given the political clout and federal affairs’ efforts of these organizations, we thought this to be a reasonable method to gauge the relative strength of the voice supporting each recommendation.
Figure 1 shows the 9 recommended modifications to the MACRA proposed rule receiving at least majority support from these 11 organizations, listed from most “votes” to fewer.
1. “Shorten ACI performance period”
Advancing Care Information (ACI) is one of the four performance categories under MACRA’s Merit-Based Incentive Payment System (MIPS) and derives measures and concepts from the Meaningful Use program. There could be as few as 60 days between the publication of the MACRA final rule and the start of the first MIPS performance year (proposed to be January 1, 2017; see #6 below). Commenters suggest reducing the first ACI performance period from 12 months down to, for instance, 90 days, so that providers have more time to prepare, as has been done for Meaningful Use in the past.
2. “Eliminate 50-clinician cap on medical home Advanced APM eligibility”
Commenters oppose the proposed rule mandating that medical home entities, such as those under the recently launched Comprehensive Primary Care Plus model (CPC+), will not qualify as Advanced Alternative Payment Model (Advanced APM) entities starting CY2018 if they are owned by organizations with more than 50 clinicians. These entities would then not receive the annual 5% Advanced APM bonus nor be exempt from MIPS.
3. “Reduce the quality data completeness threshold”
The MIPS quality category generally determines half of the MIPS score in the first performance year. The proposed “data completeness” threshold requires that clinicians report at least 90% of all patients for each quality measure, regardless of payer. Commenters feel this is too high of a reporting burden, particularly for small organizations.
4. “Reduce MIPS APM reporting requirements”
Certain APM entities are also subject to a constrained set of MIPS reporting requirements. Otherwise known as “MIPS APM” entities, CMS intended for these constrained MIPS requirements to ease reporting burdens for entities subject to both APM and MIPS programs. Commenters do not believe CMS went far enough in reducing these burdens.
5. “Raise MIPS low-volume eligibility threshold”
CMS has proposed that clinicians with fewer than $10,000 and 100 patients annually in Medicare Part B, be excluded from MIPS. Organizations, particularly those representing small practices, would like those thresholds to be raised so that more clinicians can be exempt from MIPS.
6. “Delay program start”
The proposed rule states that the first performance year will begin January 1, 2017. Commenters would like to delay the start date to July 1, 2017 and even to January 1, 2018. CMS is faced with practical challenges and legislative mandates which constrain how much the program may be delayed, however, adjustments to performance period lengths for various components of MIPS (see #1 above for ACI) may have a nearly equivalent effect to an outright delay of the entire program’s start date.
7. “Deem MSSP Track 1 ACOs as Advanced APMs or opt out of MIPS”
Medicare Shared Savings Program (MSSP) accountable care organizations (ACOs) are currently the most prevalent alternative payment models (APMs). In particular, MSSP “Track 1” ACOs comprise 90%+ of all MSSP ACOs, yet the proposed rule does not deem them to be Advanced APM entities, thereby disqualifying them from the associated annual 5% bonus and automatic exemption from MIPS. The core issue is whether Track 1 ACOs, which can earn reimbursement incentives, but cannot be assessed penalties, are bearing sufficient and appropriate financial risk according to CMS in order to earn the Advanced APM designation.
8. “Increase CPIA credit for APM participation”
The MIPS category for clinical practice improvement activities (CPIA) is 15% of the MIPS score in year 1. The proposed rule states that clinicians also participating in an APM will automatically earn a minimum of half the maximum CPIA points. Commenters request that APM participants should be granted all the maximum points for CPIA, citing the significant efforts needed to set up and run an APM entity.
9. “Reinstitute MU measure exclusions in ACI”
ACI shifts the measurement of Meaningful Use performance from a pure all-or-nothing compliance determination to a hybrid scoring system combining all-or-nothing with a continuous scoring scale. Commenters believe that the new scoring system still entails enough risk for providers, particularly in small practices, to warrant preserving the ability for some providers to gain exclusions to measures due to circumstances out of their control.
What’s Happening Now
Despite the potential for the MACRA final rule to define shorter performance periods or even a wholesale delay of the program’s start, we are not observing a slowdown in activities to prepare for MACRA. The complexity and impact of the program, combined with uncertainty about whether the above-listed modifications and others will be adopted, are causing organizations to plan for different scenarios. Meanwhile, CMS has recently published a plethora of new initiatives, such as CPC+, bundled payment models for cardiac care, and the expansion of the Medicare Diabetes Prevention Program, all which require provider organizations to analyze, decide and potentially act upon. In the midst of this period of heightened regulatory activities, it is wise to identify early which of the proposed modifications to MACRA could most impact your organization and what cross-dependencies with other CMS initiatives may exist. Stay tuned through November 1st for the release of the MACRA final rule and more clarity informing which paths to take.
Tom S. Lee, Ph.D., is the Founder and CEO of SA Ignite.
The views, opinions and positions expressed within these guest posts are those of the author alone and do not represent those of Becker’s Hospital Review/Becker’s Healthcare. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them.
