The move to an ACO model disrupts decades of process and infrastructure designed to support fee-for-service care.
As we discussed in part 1 and part 2 of this series, changing this landscape and enabling a new environment for better coordinated, more efficient delivery of care requires a clear roadmap for achieving specific quality metrics and cost savings. Charting an efficient course is likely to require new partners to deliver the technology, data analysis and population health management skills needed for success.
Whether ACO success is ultimately measured in improved care delivery and/or significant financial savings, it is not uncommon for ACOs to lack the entirety of capabilities in-house needed to design and implement a successful program. Following an exhaustive internal skills and service gap evaluation, Louisiana Physicians Accountable Care Organization (LPACO) identified a patient population that could benefit from externally provided medication management services in underserved, rural areas.
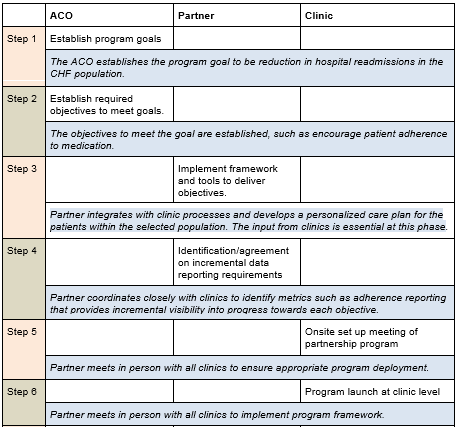
The key to building successful partnerships under the ACO model lies in clearly defining and agreeing to the requisite steps for a fully integrated partnership across the ACO. These steps must be organized in manageable increments, have clearly defined owners and partnership value delivery checkpoints.
Determining the roles of each participant
The next logical question is how to build a strong working relationship between partners, clinics and the ACO itself to ensure successful partner integration, as well as service or care delivery that meets the identified ACO objective. The answer lies in having a program plan that outlines which party should be responsible for each step.
The table below outlines an approach and includes sample steps for an ACO focused on partnering with a medication management provider to improve its quality measure for All-Cause Unplanned Admissions for Patients with Heart Failure (ACO-37):
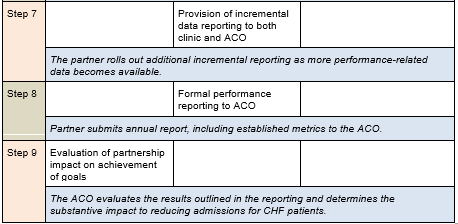
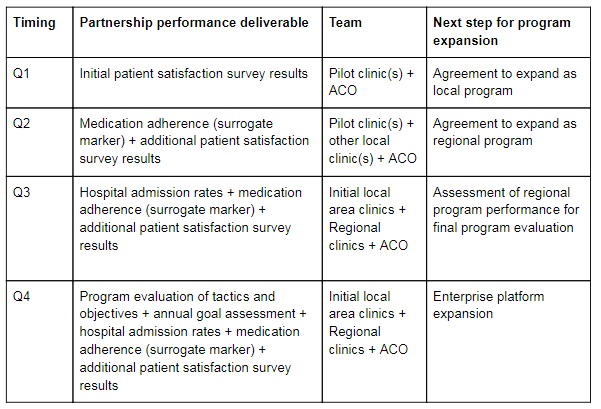
Evaluating Partner Performance
The right analytics are essential during this process to ensure that the partner relationship is evolving at a pace and a level of quality that yield not only better outcomes for patients, but measurable outcomes that assist the ACO in meeting the agreed partnership goal(s). The partner should provide input and data to clinics that guide providers in their day-to-day care of patients and that guide the ACO itself in population health decision making.
At the provider level, patient satisfaction data is a quick measure to obtain and can be used to evaluate whether continuation and expansion of the partnership are justified during the early stages of the partnership. After all, patients must be satisfied with partner performance if pilot program providers can reasonably be expected to continue the partnership and if new providers are going to willingly engage in the program.
At the clinic level, medication adherence data can help to focus the development of adherence strategies for both specific patients and selected population. An ACO might also use this information to develop tactics for addressing non-adherence across a wider spectrum of patients. Over time, utilization data such as hospital admissions can be added as a metric to clearly determine the impact of a medication management program on specific disease states. By evaluating the correlation between hospital admission rates, medication adherence rates and medication management program enrollment, it’s possible to gain measurable insight into partnership program impact.
One note: To provide a clear view of the data available to measure partner performance and to conduct ongoing analyses, the role of data analyst needs to be clearly identified as part of initial partnership discussions. It must be determined if this position can be adequately filled through someone in the ranks at the ACO, or if this skillset is best provided by a partner.
Louisiana Physicians Accountable Care Organization (LPACO) selected Curant Health as their medication management partner. Below is an example of an initial year-long engagement including the timing of specific partnership performance evaluation reviews.
In the conclusion of this series, we will share insights from one ACO using this partnership model to address internal gaps in medication adherence and data generation critical to improving care delivery and striving toward the ultimate goal of unlocking significant Medicare Shared Savings.
About the authors
Vickie Andros, PharmD, is Director of Clinical Services for Curant Health
Jake Caines is Senior Director of Commercial Strategy and Performance for Curant Health
The views, opinions and positions expressed within these guest posts are those of the author alone and do not represent those of Becker's Hospital Review/Becker's Healthcare. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them.

