Government and private insurers are gradually moving away from encounter-based reimbursement and rapidly developing new payment models that reward coordination of care and population health management. How should healthcare leaders respond? As always, there are options.
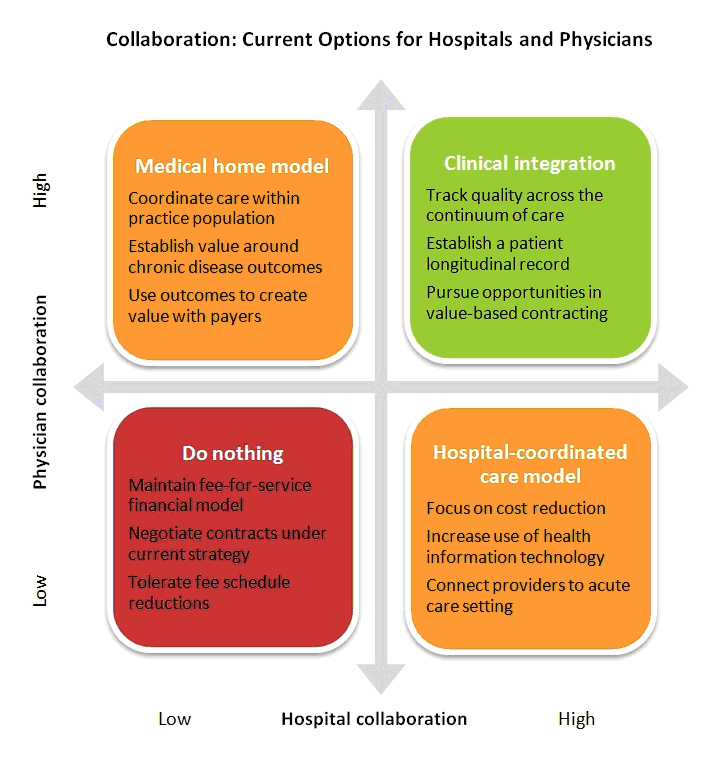
The first option is to do nothing. Both hospitals and physicians can maintain current strategies based on fee-for-service payment, avoid the up-front costs of care coordination — and tolerate declining reimbursement. Physicians will take home less pay, and hospitals will see their margins shrink.
The next option for hospitals and physicians is to work on improving care coordination, but within their respective silos. A hospital could use quality methodologies and technological tools to improve coordination of inpatient care. A physician group could develop a medical home model to coordinate care within its practice population. "Siloed coordination" will enable each party to leverage gains in payor contracting. Hospitals will be able to point to cost reductions, and physicians will be able to tout better chronic disease outcomes. The problem is that neither the hospital nor the physicians will realize the benefits of fully coordinated patient care. Their opportunities for success under value-based contracting models will be limited.
That brings us to the last option: clinical integration between hospitals and physicians. Clinical integration offers both parties the opportunity to coordinate patient interventions, manage quality across the continuum of care, move toward population health management and pursue true value-based contracting.
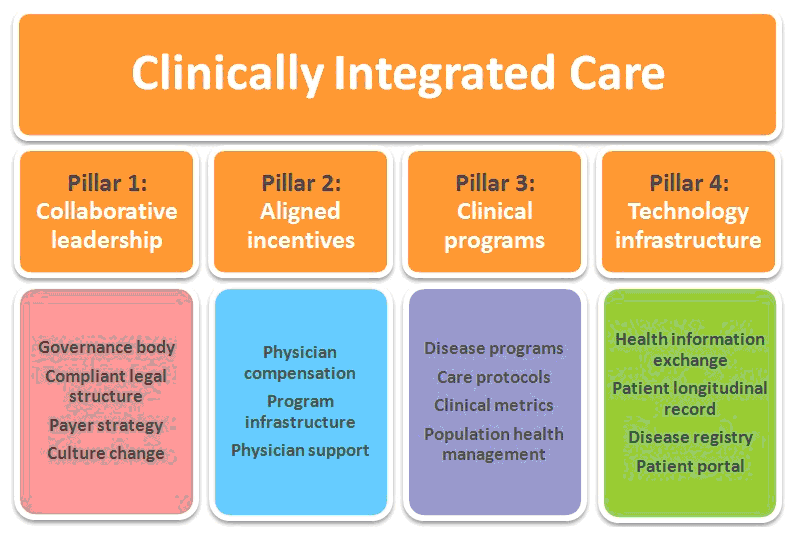
Unfortunately, the path to clinical integration is far from clear. The best strategy is to build a platform for hospital-physician collaboration that is flexible enough to support a broad range of possible futures. Right now, leading healthcare organizations are creating this versatile platform by focusing on the four "pillars" of clinical integration.
First, if a clinical integration initiative will include independent physicians, it needs to have a legal structure for contracting with payors and, in turn, paying physicians based on outcomes, not referrals. To be acceptable under Federal Trade Commission standards, a clinically integrated organization must be an independently governed entity with the objective of improving population health through coordinated programs and interventions.
Second, clinical integration requires collaboration on payor strategy. The scope goes beyond the typical Physician-Hospital Organization. The focus is on achieving clinical outcomes that can serve as value drivers within risk-based and pay-for-performance contracting models. Only a strong physician-led governance body will be able to create the clinical strategies required to pursue risk-based or value-based contracts with commercial payors, develop innovative care contracts with employers and take advantage of accountable care opportunities in the Medicare Shared Savings Program.
Third, clinical integration requires a strong physician-led governing structure for driving cultural change. For a clinically integrated organization to be successful, physicians must transition away from the fee-for-service mindset. This includes adopting new behaviors that align with outcomes-based reimbursement, such as collaborating across specialties, sharing information, managing utilization and providing proactive care. Educating providers on clinical integration concepts, including innovative care delivery models and tracking of clinical quality outcomes, is what allows community physician members to understand the value of participation.
Clearly, physician compensation is an important tool. Clinically integrated organizations must design incentive plans that not only encourage productivity, but reward physician efforts to achieve shared goals in care, quality and cost control.
But compensation design is not enough to ensure strong performance. Organizations need to create support structures to help physicians understand and work toward performance objectives:
Supporting all of these efforts, leaders need to build a financial infrastructure to guide overall decision making. One key priority is to develop a risk-based cost model that links patient care costs to interventions and quality outcomes. Finance leaders will also need to begin engaging with payors to explore and negotiate risk-based contracts and develop a physician performance incentive fund.
To launch a care coordination strategy, begin by creating clinical programs that target major opportunities in care improvement. Initial areas of concentration may include:
The next step is to develop appropriate clinical performance measures. For example, an asthma care program could track asthma control rates, screening frequency and percentage of patients with an up-to-date asthma action plan. The program could also track cost measures such as drug expenses, physician visits and emergency room visits.
Clinical programs should also develop care plans that define care protocols for various conditions. Program leaders can use process mapping to create care pathways that encompass ambulatory, inpatient, post-acute and home health interventions. Care gaps reports can be created to identify opportunities to enhance delivery of patient care according to care protocols and measure clinical care performance by care setting.
Physicians who are used to encounter-based reimbursement need guidance on how to be successful within a clinically integrated initiative. Support should focus on helping physicians manage patients within care plans through the use of care coaches and care coordination tools. Many physicians will also need coaching on how to incorporate nurses, dietitians and other support providers into care efforts aimed at managing the patient outside the traditional office setting.
Proactive medicine is key. Traditionally, a physician knows that a patient has a problem only when the patient comes in for an appointment. The success of clinical integration will hinge on physicians' ability to anticipate and prevent patient problems. To do this, physicians will need to incorporate care gap reports into clinical care and adopt new processes — for example, assigning a nurse to call patients with high-risk diabetes to ensure hemoglobin A1C is reported according to the defined diabetic clinical treatment protocol.
The first priority is to invest in technologies that support coordination of care. One approach is to develop a health information exchange that connects ambulatory electronic medical records (of both employed and independent physicians), the hospital EMR, pharmacy information systems, labs, etc. The goal is to create a patient longitudinal record that allows physicians, nurses and other providers across the care community to track patient care in every setting.
Next, begin investing in technologies that support population health management. A clinically integrated organization needs to be able to aggregate and analyze clinical data so it can identify performance shortfalls and strategize improvements. Stage 1 meaningful use data from the ambulatory EMR and Physician Quality Reporting System can serve as a starting point, but to achieve significant gains in quality and cost, the organization needs comprehensive clinical and claims data from disparate information systems. The solution is to create a disease registry, a database that enables an organization to capture information from various provider systems and sources. The key is to incorporate a tool that allows the clinically integrated organization to run performance analytics on clinical programs, care settings, provider performance and cost utilization.
Clinically integrated organizations should also invest in technologies for connecting patients. Patient electronic engagement — via patient portals and secure messaging — is a requirement under stage 2 meaningful use. Beyond the requirements, organizations should explore patient portal and personal health record technologies for involving patients more deeply in clinical programs.
For example, a clinically integrated organization might set the goal of reducing high-risk diabetic patients from 12 percent to 8 percent of its patient population, compared to a community-wide rate of 10 percent. If the organization can achieve this outcome and demonstrate it with valid data, it will be in a position to negotiate favorable risk-based or shared savings performance contracts that enhance revenue and drive patient volume.
None of these pillars can be built overnight, but leading organizations are making steady headway in each area. Clinical integration is not a project with a defined endpoint, but an evolution that will require ongoing attention, quality improvement, resources and leadership.
Daniel J. Marino is the president and CEO of Health Directions, a national consulting firm that provides business solutions for healthcare organizations. He can be reached at (312) 396-5400 or dmarino@healthdirections.com.
Clinical Integration: A Joint Physician-Hospital Strategy to Enhance the Value of Care
5 Lessons Learned From a Clinical Integration Expert
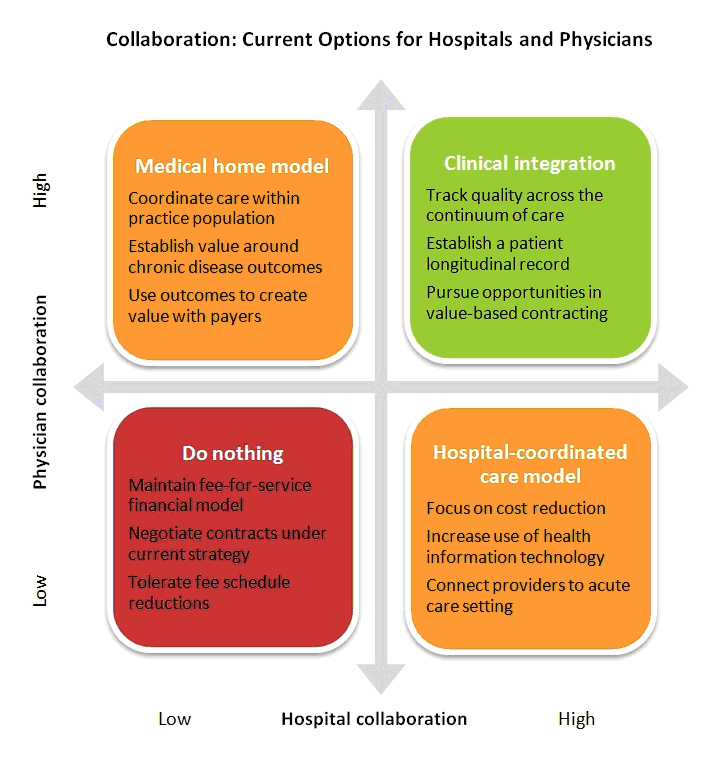
The first option is to do nothing. Both hospitals and physicians can maintain current strategies based on fee-for-service payment, avoid the up-front costs of care coordination — and tolerate declining reimbursement. Physicians will take home less pay, and hospitals will see their margins shrink.
The next option for hospitals and physicians is to work on improving care coordination, but within their respective silos. A hospital could use quality methodologies and technological tools to improve coordination of inpatient care. A physician group could develop a medical home model to coordinate care within its practice population. "Siloed coordination" will enable each party to leverage gains in payor contracting. Hospitals will be able to point to cost reductions, and physicians will be able to tout better chronic disease outcomes. The problem is that neither the hospital nor the physicians will realize the benefits of fully coordinated patient care. Their opportunities for success under value-based contracting models will be limited.
That brings us to the last option: clinical integration between hospitals and physicians. Clinical integration offers both parties the opportunity to coordinate patient interventions, manage quality across the continuum of care, move toward population health management and pursue true value-based contracting.
Unfortunately, the path to clinical integration is far from clear. The best strategy is to build a platform for hospital-physician collaboration that is flexible enough to support a broad range of possible futures. Right now, leading healthcare organizations are creating this versatile platform by focusing on the four "pillars" of clinical integration.
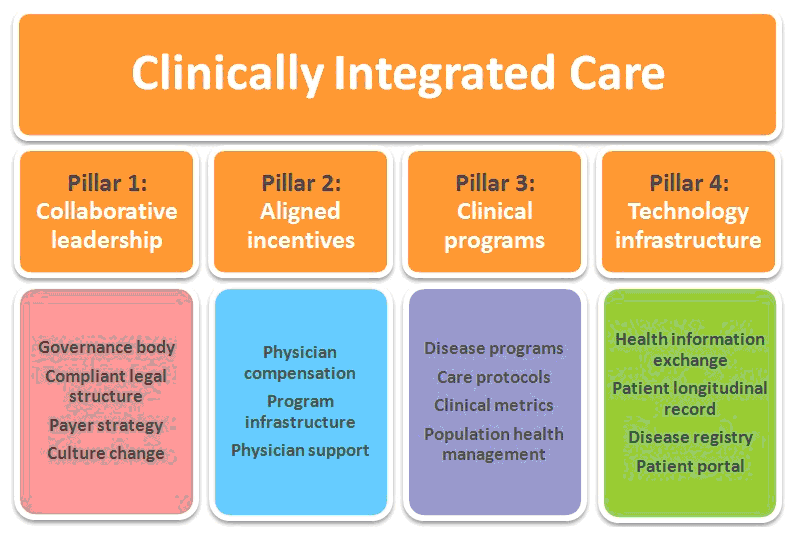
1. Collaborative leadership
The first pillar of clinical integration is a shared governance body with strong physician leadership. Getting governance right is critical for three reasons.First, if a clinical integration initiative will include independent physicians, it needs to have a legal structure for contracting with payors and, in turn, paying physicians based on outcomes, not referrals. To be acceptable under Federal Trade Commission standards, a clinically integrated organization must be an independently governed entity with the objective of improving population health through coordinated programs and interventions.
Second, clinical integration requires collaboration on payor strategy. The scope goes beyond the typical Physician-Hospital Organization. The focus is on achieving clinical outcomes that can serve as value drivers within risk-based and pay-for-performance contracting models. Only a strong physician-led governance body will be able to create the clinical strategies required to pursue risk-based or value-based contracts with commercial payors, develop innovative care contracts with employers and take advantage of accountable care opportunities in the Medicare Shared Savings Program.
Third, clinical integration requires a strong physician-led governing structure for driving cultural change. For a clinically integrated organization to be successful, physicians must transition away from the fee-for-service mindset. This includes adopting new behaviors that align with outcomes-based reimbursement, such as collaborating across specialties, sharing information, managing utilization and providing proactive care. Educating providers on clinical integration concepts, including innovative care delivery models and tracking of clinical quality outcomes, is what allows community physician members to understand the value of participation.
2. Aligned incentives
Hospitals and physicians share many goals, but their priorities often diverge. It is essential that clinically integrated organizations develop structures that align goals and incentives across the entire spectrum of providers.Clearly, physician compensation is an important tool. Clinically integrated organizations must design incentive plans that not only encourage productivity, but reward physician efforts to achieve shared goals in care, quality and cost control.
But compensation design is not enough to ensure strong performance. Organizations need to create support structures to help physicians understand and work toward performance objectives:
- Develop a plan for communicating strategies and decisions to the entire organization.
- Assign staff and resources to physician education and office staff training.
- Develop a provider scorecard that keeps physicians oriented toward improving clinical outcomes and controlling costs.
Supporting all of these efforts, leaders need to build a financial infrastructure to guide overall decision making. One key priority is to develop a risk-based cost model that links patient care costs to interventions and quality outcomes. Finance leaders will also need to begin engaging with payors to explore and negotiate risk-based contracts and develop a physician performance incentive fund.
3. Clinical programs
The heart of clinical integration is care coordination. Greater coordination between providers will improve patient outcomes and wring costs out of the system by optimizing care transitions, reducing redundant testing and providing better management of patients with multiple complex co-morbidities and diagnoses.To launch a care coordination strategy, begin by creating clinical programs that target major opportunities in care improvement. Initial areas of concentration may include:
- High-risk patients (for example, diabetics with multiple co-morbidities such as hypertension or heart failure)
- Cost-control opportunities (like generic prescribing and MRI utilization review)
- Key public health initiatives (such as smoking cessation and depression screening)
The next step is to develop appropriate clinical performance measures. For example, an asthma care program could track asthma control rates, screening frequency and percentage of patients with an up-to-date asthma action plan. The program could also track cost measures such as drug expenses, physician visits and emergency room visits.
Clinical programs should also develop care plans that define care protocols for various conditions. Program leaders can use process mapping to create care pathways that encompass ambulatory, inpatient, post-acute and home health interventions. Care gaps reports can be created to identify opportunities to enhance delivery of patient care according to care protocols and measure clinical care performance by care setting.
Physicians who are used to encounter-based reimbursement need guidance on how to be successful within a clinically integrated initiative. Support should focus on helping physicians manage patients within care plans through the use of care coaches and care coordination tools. Many physicians will also need coaching on how to incorporate nurses, dietitians and other support providers into care efforts aimed at managing the patient outside the traditional office setting.
Proactive medicine is key. Traditionally, a physician knows that a patient has a problem only when the patient comes in for an appointment. The success of clinical integration will hinge on physicians' ability to anticipate and prevent patient problems. To do this, physicians will need to incorporate care gap reports into clinical care and adopt new processes — for example, assigning a nurse to call patients with high-risk diabetes to ensure hemoglobin A1C is reported according to the defined diabetic clinical treatment protocol.
4. Technology infrastructure
New connectivity and point-of-care tools make hospital-physician collaboration more possible than ever. The risk is overspending on technology and under-delivering on functionality. The key to avoiding these problems is to create a focused IT investment strategy.The first priority is to invest in technologies that support coordination of care. One approach is to develop a health information exchange that connects ambulatory electronic medical records (of both employed and independent physicians), the hospital EMR, pharmacy information systems, labs, etc. The goal is to create a patient longitudinal record that allows physicians, nurses and other providers across the care community to track patient care in every setting.
Next, begin investing in technologies that support population health management. A clinically integrated organization needs to be able to aggregate and analyze clinical data so it can identify performance shortfalls and strategize improvements. Stage 1 meaningful use data from the ambulatory EMR and Physician Quality Reporting System can serve as a starting point, but to achieve significant gains in quality and cost, the organization needs comprehensive clinical and claims data from disparate information systems. The solution is to create a disease registry, a database that enables an organization to capture information from various provider systems and sources. The key is to incorporate a tool that allows the clinically integrated organization to run performance analytics on clinical programs, care settings, provider performance and cost utilization.
Clinically integrated organizations should also invest in technologies for connecting patients. Patient electronic engagement — via patient portals and secure messaging — is a requirement under stage 2 meaningful use. Beyond the requirements, organizations should explore patient portal and personal health record technologies for involving patients more deeply in clinical programs.
Tying it all together
The overall goal of the four-pillar platform is to link clinical outcomes to cost management with the aim of negotiating value-based payor contracts. In light of this goal, clinically integrated organizations need to be able to aggregate data for the entire network and compare outcomes to community performance.For example, a clinically integrated organization might set the goal of reducing high-risk diabetic patients from 12 percent to 8 percent of its patient population, compared to a community-wide rate of 10 percent. If the organization can achieve this outcome and demonstrate it with valid data, it will be in a position to negotiate favorable risk-based or shared savings performance contracts that enhance revenue and drive patient volume.
Looking ahead
While both hospitals and physicians have several options for taking advantage of new payment models, clinical integration represents the best opportunity for both parties. The key to success is a flexible strategy that emphasizes effective governance, aligned incentives, clinical programs and appropriate technology.None of these pillars can be built overnight, but leading organizations are making steady headway in each area. Clinical integration is not a project with a defined endpoint, but an evolution that will require ongoing attention, quality improvement, resources and leadership.
Daniel J. Marino is the president and CEO of Health Directions, a national consulting firm that provides business solutions for healthcare organizations. He can be reached at (312) 396-5400 or dmarino@healthdirections.com.
More Articles on Clinical Integration:
The 7 Components of a Clinical Integration NetworkClinical Integration: A Joint Physician-Hospital Strategy to Enhance the Value of Care
5 Lessons Learned From a Clinical Integration Expert

