To effectively position for the future realities of healthcare while maintaining focus on current operations, many hospitals and physicians are turning to clinical integration as a viable option to (1) increase quality, (2) reduce cost and waste in the current system to maintain margins, (3) sustain independence for physicians not ready for hospital employment and (4) position providers to take on higher levels of accountability to effectively manage utilization and the health of populations in the future.
CI is commonly defined as a health network working together, using proven protocols and measures, to improve patient care, decrease cost and demonstrate value to the market. Once the CI network can demonstrate a value proposition, payors and large employers are approached to support the network and other incentives that are based on achieving defined results. In most cases, CI networks and the initial conversations with payors are initiated by health systems. However, to be successful, CI networks must become physician-led, professionally managed organizations.
Organizations should keep the Federal Trade Commission’s clinical integration definition and requirements in mind during CI program development and implementation. In 1996, the Department of Justice and the FTC defined CI as an active and ongoing program to evaluate and modify practice patterns by the CI network’s physician participants and create a high degree of interdependence and cooperation among the physicians to control costs and ensure quality. Generally, the FTC considers a program to be clinically integrated if it performs the following:
- Establishes mechanisms to monitor and control utilization of healthcare services that are designed to control costs and ensure quality of care.
- Selectively chooses CI network physicians who are likely to further these efficiency objectives.
- Utilizes investment of significant capital, both monetary and human, in the necessary infrastructure and capability to realize the claimed efficiencies.
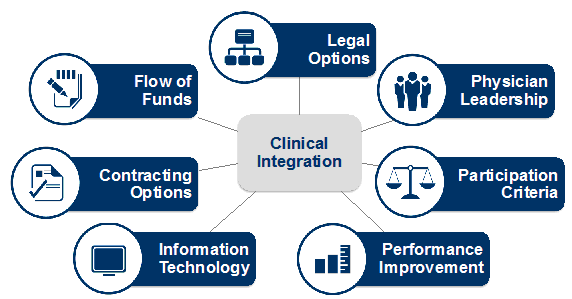
7 Components
To effectively implement CI, the network should understand the relevance and the possible options for each of the seven components discussed below.
1. Legal options. To legally implement CI, the health system and physicians are required to organize in a structure that supports program objectives. With the exception of an employment-only model, a CI network can primarily be created within a (an):
- Physician-hospital organization — A joint venture between a health system and its medical staffs.
- Independent practice association — Owned and operated by only physician partners.
- Subsidiary of the health system — The health system is the sole corporate member of the subsidiary entity and member physicians sign separate legal agreements to participate.
Traditionally these structures have been used to negotiate and handle managed care contracts (HMO, fee-for-fervice, etc.) for a defined network of providers and they are now being utilized as the vehicle to implement CI networks by achieving the following objectives:
- Establishing a network of providers that enables enhanced coordination of care.
- Creating a new partnership model with employed and independent physicians that includes defined roles for physician leadership.
- Defining performance improvement initiatives to provide demonstrated value to the market.
- Providing a platform for joint contracting to support care redesign and performance improvement initiatives.
- Negotiating with potential partners for risk-based contracts.
Each legal option is capable of achieving these CI objectives and they differ in ownership structure and capitalization requirements. Some hospitals and physicians already have a PHO or IPA in place and are using those entities as the foundation for their CI programs. For example, a four-hospital system in the Midwest chose to utilize a PHO as their vehicle for CI because the business entity was already created. Although the infrastructure was not entirely created to support a fully-functioning CI network, the PHO created an opportunity for ownership, access to resources, strong public perception and the analytics staff to support quality programs. However, to limit physician costs while still allowing physicians to have a significant leadership role in the network; a four-hospital system in the southeast created a subsidiary of the health system to launch its program.
2. Physician leadership. Integration in the post-reform era requires a high degree of physician-hospital alignment that is based on trust and transparency. Health systems willing to pursue CI must empower physician leaders to have an influence on the future direction of the CI network. This will help to integrate the physician’s clinical expertise into hospital operations and also increase cooperation and credibility of the CI network. Furthermore, dedicated physicians and administrative leadership will be required to successfully implement a major change project of this magnitude.
A vital step to physician engagement and leadership is a robust communication strategy across the network and its partners. Clear goals and objectives by both employed and independent physicians will encourage dialogue and partnership formation as the strategy is implemented.
Once the CI network is created, a governance structure should be developed. Physician leaders should participate on the CI board and provide leadership to committees formed to achieve program objectives. Other participating physicians may lead and/or participate on sub-committees supported by the CI network or health system. CI committees may merge with existing committees in place within the health system (i.e., executive committee, quality committee and contracting committee).
3. Participation criteria. Member physicians or groups in the CI network must sign a participation agreement. This agreement outlines the expectations and requirements for participation in the CI program. In the initial stages of the network, it is very critical that member physicians adhere to program guidelines to help ensure that stated objectives are met and the network’s value proposition is able to be demonstrated to the market.
Recognizing this, one large CI network in the Southeast included information technology adoption in the participation criteria to ensure that the network was able to demonstrate the value of enhanced coordination between providers following evidence-based guidelines. To ingrain IT utilization into the culture, not only did the CI network initially include IT adoption and utilization in the participation criteria, but the network also designated a portion of the performance incentive dollars to this area to increase compliance.
As the network matures and the participation criteria is solidified into the culture, incentive payments are not typically awarded for compliance. However, to keep physicians focused on program requirements, physician eligibility in the incentive program may be tied to meeting the participation criteria.
Sample participation criteria include:
- Maintaining the appropriate IT infrastructure.
- Logging into the CI Network website to view network and individual performance.
- Compliance with clinical protocols and care pathways developed by the network.
- Participation in all network contracts.
4. Performance improvement. Clinical quality and operational improvement projects are necessary components of a CI program. CI provides a vehicle that engages physicians in determining how quality is defined and measured. CI also allows physicians to take an active role in care redesign and protocol development to increase quality, more effectively manage costs, reduce variation and eliminate unnecessary waste within the delivery system. The performance initiatives span across specialties and sites of care.
To achieve performance improvement, the CI network works to define baseline performance and identify areas where the network can demonstrate quality and operational efficiencies to the market. It is critical that physicians play an active role in selecting metrics for the performance improvement initiatives. CI networks should select performance improvement initiatives based on the (1) feasibility of capturing sufficient data to monitor performance, (2) improvement opportunity, (3) payor, employer and/or hospital interest in the program and (4) the ability of participating physicians to impact the targeted metrics.
Performance improvement initiatives can be complex and difficult to monitor effectively based on the sophistication of the network’s IT system and the capacity of the network to manage multiple initiatives effectively. Recognizing this, one large multi-hospital system in the Midwest implemented their initiatives in a phased approach over time and ensured that all metrics were consistent across contracts. Individual metrics were then reevaluated and updated on an annual basis to help ensure that the initiatives continued to demonstrate the value of the network. Performance improvement initiatives are typically developed in the following categories:
- Variance and cost reduction — Improving operational efficiencies
- Clinical efficiency — Reducing avoidable, unproductive and duplicative services
- Care redesign — Ensuring treatment in the most optimal setting and by the right provider
- System optimization — Shifting focus to preventive care and population health
- Patient experience —Objective and meaningful comparisons between providers of care
5. Information technology. If you do not measure it, you cannot improve it. IT is the backbone of the CI network’s value proposition and is critical to improving coordination and connectivity between providers of care. Early adopters of CI would manually input data and transfer information by excel template report cards. Today the industry is inundated with tools to assist with monitoring and reporting the care provided to a patient. Since providers will be affected most by a change in technology, they must be heavily involved in choosing the correct vendor. Two types of data sharing sources being used most by hospitals are electronic health records and patient registries. However, health information exchanges are becoming more popular and could eventually become robust enough to support clinically integrated initiatives.
An EHR is a medical record for a patient in a physician office, hospital, ancillary care facility or ambulatory care facility. The EHR is intended to replace paper-based patient records for recording encounter-based information on each patient who receives care from the provider entity and includes electronic: data entry, order entry, prescribing and transcription.
A patient registry is a repository that holds clinical information specific to a disease, disease process, implant, drug, etc. A cancer registry is an example of a disease-specific database. The registry is intended to track (1) patients and their compliance with specific chronic disease (or wellness) based guidelines across populations, (2) physician compliance with those guidelines and (3) outcomes for specific interventions. A data registry differentiates itself by interfaces with multiple data sources to provide sufficient data at the point of care provided to a patient, which is why many CI networks are utilizing data registries as opposed to the electronic medical records approach.
6. Contracting options. The purpose of CI is to provide higher quality care. Creating a CI network for the sole purpose of negotiating better rates is not the purpose of CI. However, CI networks are rewarded for demonstrated value, which is defined as the highest quality care at the lowest cost.
The CI network can contract with payors, employers or health systems. These contracts can range from a specific procedure to a population of patients. Many hospital systems have reported that payors are not requiring that CI contracts include downside risk for the network. A six-hospital system in the Southeast reported that a major payor has approached them with a contracting model that would reward their network for demonstrated performance in the following ways:
- Premium base rates — Increased fee-for-service rates based on expected performance
- Performance incentives — Incentive payments made for performance improvement initiatives
- Shared savings — Savings shared based on a reduction in the cost of care
Some hospitals have also contracted with their own CI network to realize cost saving opportunities and to more effectively manage cost within their own health plan. A hospital system in the Southwest has implemented this strategy. The savings that are generated by the network are shared to fund the CI program and to make distributions to member physicians.
7. Flow of funds. Calculation and distribution of CI incentives to physicians and to the health system occur after performance is achieved. A distribution of funds will typically be realized through cost savings, quality and efficiency programs negotiated by the CI network and its partners. Funds are distributed based on meeting performance objectives and performance can be defined in a variety of ways. For example, some CI networks reward simply for global network compliance of the CI agreement while other CI networks reward based on site (multiple hospital systems), specialty and individual performance.
Regardless of how the funds flow to the members of the CI network, the methodology should be transparent and easy to understand. Key considerations for CI network distribution methodologies include:
- Distribute rewards based on measurable performance.
- Reduce complexity of distribution methodology.
- Increase transparency across the network.
Conclusion
Health systems and physicians are implementing CI networks across the nation to respond to changing healthcare dynamics that are holding providers more accountable for quality and outcomes. Each CI network needs to create a disciplined approach to assessing and developing the key components of their network to create a sufficient value proposition for the health system, physicians, payers and employers. As CI becomes a strategic imperative in most markets, organizations should keep the following critical success factors in mind to accelerate the implementation of a successful and sustainable CI network:
- Align your health system objectives with the CI vision and strategy to avoid conflicting messages in your market.
- Involve physician leaders in the CI development process to gain physician buy-in for program objectives.
- Express a willingness to create a new partnership model with employed and independent physicians that includes defined roles for physician leadership.
- Maintain systems that can track and monitor clinical data across the continuum of ambulatory, acute and post-acute services.
- Utilize a scaled approach to develop a comprehensive list of metrics that provide value to multiple stakeholders and positions the CI network for greater levels of accountability.
- Create an effective communication strategy across all stakeholders to increase understanding of the key issues of CI.
- Commit to approach payers in the market as a combined network.
Michael Strilesky is a manager with Dixon Hughes Goodman, where he develops strategic and operational solutions for healthcare clients. Mr. Strilesky can be reached at michael.strilesky@dhgllp.com.
More Articles on Clinical Integration:
Ideas Into Action: 3 Hospital CEOs Talk Strategy Going Into 2013
Strategies for Facing the Accelerating Transformation of U.S. Healthcare
