Sky Lakes Medical Center, located in Klamath Falls, Ore., does not turn patients away. An isolated community hospital serving 100,000 people within a 10,000-square-mile area, the medical center takes "all comers." To accompany its mission of "consistently offering competent care sensitively delivered to all who enter its doors," Sky Lakes has developed a robust financial assistance policy.
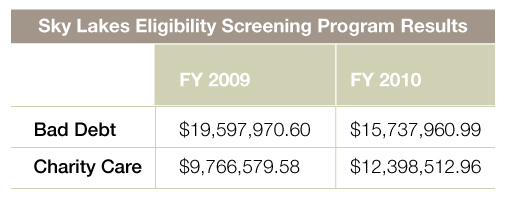
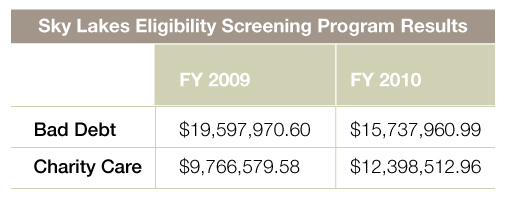
There is no doubt that Sky Lakes cares whole-heartedly for its community. In fiscal year 2010, it provided more than $12 million in charity care. But, feeling the strain of a weak economy like so many healthcare organizations, the medical center also wrote off nearly $16 million in bad debt. As heavy as that burden was, however, it was nevertheless lighter than the previous year’s bad debt load of $19.6 million.
Sky Lakes’ improved financial standing is a testament to a concerted effort to fortify itself against the poor economy while offering care to all. The medical center knew that to continue providing benefits to the region, it needed a strategy to strengthen its own bottom line.
Reinforcing the revenue cycle
The 501(c)3 regional healthcare center is licensed for 176 beds and offers financial relief for thousands of patients. Sky Lakes' assistance policy offers options to families earning up to four times the federal poverty level , meaning individuals in need can get the care they deserve without worrying about high costs. In addition, medical center leadership has established maximum out-of-pocket limits for qualifying patients. For example, the maximum out-of-pocket expense for a patient earning 350 to 400 percent of the FPL is $25,000, while those with an annual income of up to twice the FPL receive care at no cost.

As expected, offering such a community-forward program is not without cost. The financial burden of providing uncompensated care is one of the major issues for Sky Lakes and many hospitals.
It is commonly understood by hospitals nationwide that many uninsured patients are not aware they qualify for various government-sponsored coverage, such as Medicaid and Social Security Disability Insurance. Because of this, organizations often host state Department of Health and Human Services workers or train in-house staff to screen uninsured patients for eligibility. Sky Lakes, prior to 2009, hosted social workers from the Oregon Health Plan who would assist the medical center in filling applications for self-pay individuals. But it wasn’t enough.
With the poor economy, Sky Lakes saw more uninsured walking through its doors. While many would, of course, qualify for its financial assistance program, the medical center knew many of these patients were also likely to be eligible for Medicaid or SSDI. Additionally, to ensure the future viability of its generous patient-aid benefit, leadership needed to reduce its exposure to uncompensated care. The medical center fully understands that when individuals delay medical care, it does not only affect the organization’s bottom line, but it also has long-term impacts on the health of the entire community.
Sky Lakes knew that if it could amplify its efforts to screen patients and help them apply for Medicaid and other programs, it could likely increase reimbursement for care. In turn, this would allow the medical center to support more patients with its financial assistance program. The organization lacked the staff to dedicate to full-time eligibility services, however, and realized that the ongoing training of in-house personnel would be a major strain on resources.
After evaluating its options, Sky Lakes turned to examining consultant firms specializing in the screening and application for federal and state coverage programs. Leadership has high standards for its staff and associates, so stringent expectations were set. Knowing that bringing on an outside company can be disruptive to internal processes, the medical center determined several requirements. Consultants must:
• work on-site with patients,
• not collect payment or charge a fee for services to patients,
• have the mindset that they were providing a service to the uninsured,
• be comfortable working directly with nursing staff, and
• hit the ground running with current program knowledge and professionalism.
In 2009, the medical center partnered with a firm that brought two specialists into the hospital to work face-to-face with uninsured patients. The selected consultant, Chamberlin Edmonds, an Emdeon company, does not charge patients for coverage screening services.
Putting the program in place
Leadership was aware that the consultants needed to be integrated with the medical center staff in a sensitive manner. In order to introduce the newcomers and their roles, Sky Lakes presented the specialists as patient advocates who would be working side-by-side with in-house personnel. Clinical and administrative staff were made aware of the fact that, if coverage was secured for more patients, then the organization could continue to provide the best care to all those in need.
A round-table discussion was held with eligibility specialists and various department groups to craft processes and expectations. Medical center representatives determined that the consultants would interact directly with nursing and admissions staff to identify uninsured patients on a day-to-day basis. Eligibility specialists would handle referrals from both in- and out-patient departments, and then personally interview individuals and assist them throughout the application process.
At the start of the partnership, Sky Lakes sent a large number of existing patient accounts to the specialists. Each account included in the initial screening was no more than 90 days old. The intent was to secure retroactive coverage for patients who may qualify for Medicaid or SSDI, as Medicaid’s policy is to reimburse providers for healthcare services administered no more than 90 days prior to the date of application. The consultants worked to obtain approval on these accounts, which would have otherwise been classified as uncompensated care. Between October 2009 and February 2010, Chamberlin Edmonds was successful in qualifying 266 patients for benefits—patients whose then-current and outstanding medical bills totaled almost $3 million.
Results of a patient-forward program
Thus far, the eligibility screening program has far exceeded the medical center’s expectations. During fiscal year 2010, specialists secured Medicaid reimbursement for $814,209 worth of care provided to the uninsured—at no cost to the patients. Compared to fiscal year 2009 — which carried a bad debt load of $19,597,970 — 2010 saw a reduction of nearly $4 million for a total of $15,737,960.
For the staff of Sky Lakes, bringing in an eligibility consulting firm was not about the increased revenue, it was about helping patients. As a result of the screening program, the medical center was able to provide an additional $2.5 million in charity care during fiscal year 2010 for a total of $12,398,512. Teaming with the consultants has given otherwise uninsured patients coverage that stays with them beyond the walls of the medical center and allows the organization the freedom to help additional individuals in need.
The Sky Lakes philosophy is “Life: Healing: Peace.” With the new services available to patients, the medical center is making great strides in helping individuals find a little more of that peace.
Learn more about Sky Lakes Medical Center.
Related articles on Medicaid:
More Than Half of States Expanded Medicaid Programs in 2010
There is no doubt that Sky Lakes cares whole-heartedly for its community. In fiscal year 2010, it provided more than $12 million in charity care. But, feeling the strain of a weak economy like so many healthcare organizations, the medical center also wrote off nearly $16 million in bad debt. As heavy as that burden was, however, it was nevertheless lighter than the previous year’s bad debt load of $19.6 million.
Sky Lakes’ improved financial standing is a testament to a concerted effort to fortify itself against the poor economy while offering care to all. The medical center knew that to continue providing benefits to the region, it needed a strategy to strengthen its own bottom line.
Reinforcing the revenue cycle
The 501(c)3 regional healthcare center is licensed for 176 beds and offers financial relief for thousands of patients. Sky Lakes' assistance policy offers options to families earning up to four times the federal poverty level , meaning individuals in need can get the care they deserve without worrying about high costs. In addition, medical center leadership has established maximum out-of-pocket limits for qualifying patients. For example, the maximum out-of-pocket expense for a patient earning 350 to 400 percent of the FPL is $25,000, while those with an annual income of up to twice the FPL receive care at no cost.

As expected, offering such a community-forward program is not without cost. The financial burden of providing uncompensated care is one of the major issues for Sky Lakes and many hospitals.
It is commonly understood by hospitals nationwide that many uninsured patients are not aware they qualify for various government-sponsored coverage, such as Medicaid and Social Security Disability Insurance. Because of this, organizations often host state Department of Health and Human Services workers or train in-house staff to screen uninsured patients for eligibility. Sky Lakes, prior to 2009, hosted social workers from the Oregon Health Plan who would assist the medical center in filling applications for self-pay individuals. But it wasn’t enough.
With the poor economy, Sky Lakes saw more uninsured walking through its doors. While many would, of course, qualify for its financial assistance program, the medical center knew many of these patients were also likely to be eligible for Medicaid or SSDI. Additionally, to ensure the future viability of its generous patient-aid benefit, leadership needed to reduce its exposure to uncompensated care. The medical center fully understands that when individuals delay medical care, it does not only affect the organization’s bottom line, but it also has long-term impacts on the health of the entire community.
Sky Lakes knew that if it could amplify its efforts to screen patients and help them apply for Medicaid and other programs, it could likely increase reimbursement for care. In turn, this would allow the medical center to support more patients with its financial assistance program. The organization lacked the staff to dedicate to full-time eligibility services, however, and realized that the ongoing training of in-house personnel would be a major strain on resources.
After evaluating its options, Sky Lakes turned to examining consultant firms specializing in the screening and application for federal and state coverage programs. Leadership has high standards for its staff and associates, so stringent expectations were set. Knowing that bringing on an outside company can be disruptive to internal processes, the medical center determined several requirements. Consultants must:
• work on-site with patients,
• not collect payment or charge a fee for services to patients,
• have the mindset that they were providing a service to the uninsured,
• be comfortable working directly with nursing staff, and
• hit the ground running with current program knowledge and professionalism.
In 2009, the medical center partnered with a firm that brought two specialists into the hospital to work face-to-face with uninsured patients. The selected consultant, Chamberlin Edmonds, an Emdeon company, does not charge patients for coverage screening services.
Putting the program in place
Leadership was aware that the consultants needed to be integrated with the medical center staff in a sensitive manner. In order to introduce the newcomers and their roles, Sky Lakes presented the specialists as patient advocates who would be working side-by-side with in-house personnel. Clinical and administrative staff were made aware of the fact that, if coverage was secured for more patients, then the organization could continue to provide the best care to all those in need.
A round-table discussion was held with eligibility specialists and various department groups to craft processes and expectations. Medical center representatives determined that the consultants would interact directly with nursing and admissions staff to identify uninsured patients on a day-to-day basis. Eligibility specialists would handle referrals from both in- and out-patient departments, and then personally interview individuals and assist them throughout the application process.
At the start of the partnership, Sky Lakes sent a large number of existing patient accounts to the specialists. Each account included in the initial screening was no more than 90 days old. The intent was to secure retroactive coverage for patients who may qualify for Medicaid or SSDI, as Medicaid’s policy is to reimburse providers for healthcare services administered no more than 90 days prior to the date of application. The consultants worked to obtain approval on these accounts, which would have otherwise been classified as uncompensated care. Between October 2009 and February 2010, Chamberlin Edmonds was successful in qualifying 266 patients for benefits—patients whose then-current and outstanding medical bills totaled almost $3 million.
Results of a patient-forward program
Thus far, the eligibility screening program has far exceeded the medical center’s expectations. During fiscal year 2010, specialists secured Medicaid reimbursement for $814,209 worth of care provided to the uninsured—at no cost to the patients. Compared to fiscal year 2009 — which carried a bad debt load of $19,597,970 — 2010 saw a reduction of nearly $4 million for a total of $15,737,960.
For the staff of Sky Lakes, bringing in an eligibility consulting firm was not about the increased revenue, it was about helping patients. As a result of the screening program, the medical center was able to provide an additional $2.5 million in charity care during fiscal year 2010 for a total of $12,398,512. Teaming with the consultants has given otherwise uninsured patients coverage that stays with them beyond the walls of the medical center and allows the organization the freedom to help additional individuals in need.
The Sky Lakes philosophy is “Life: Healing: Peace.” With the new services available to patients, the medical center is making great strides in helping individuals find a little more of that peace.
Learn more about Sky Lakes Medical Center.
Related articles on Medicaid:
More Than Half of States Expanded Medicaid Programs in 2010

