I have been reading articles recently in which CFO’s across the industry are taking a stance to maintain the pay for volume strategy in order to maintain the certainty of their revenue stream for as long as possible in this evolving reimbursement environment. It may be a sound strategy for today BUT there is value based revenue available NOW! that will facilitate the necessary transition from volume to value.
In addition to all of the traditional revenue available for volume, there are current reimbursement models that could be implemented to support a gradual transition from volume to value and still maintain current volume based revenue. The Medicare Wellness Program is a great example of one such program. Medicare Wellness is a program that supports improved wellness for patients, VALUE, through a comprehensive health risk assessment that is performed largely by the clinical support staff with a provider reviewing the assessment with the patient for approximately only 10 minutes of the entire 45 minute visit. The reimbursement for these visits averages $170 for the annual wellness visit in the first two years of eligibility and average $117 in subsequent annual wellness visits.
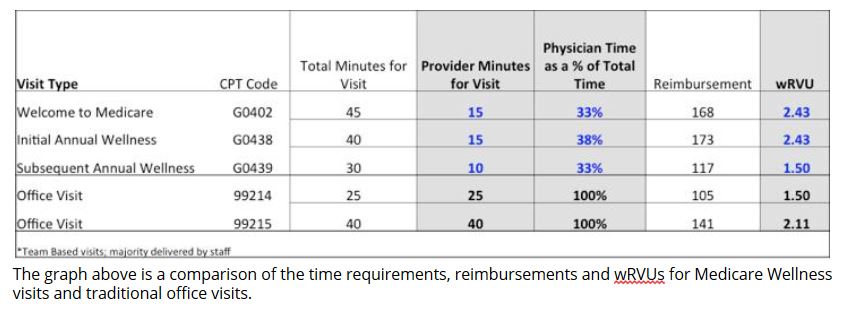
Medicare Wellness is a program that was approved ten years ago yet there continues to be minimal penetration of not greater than 15% in most markets. The biggest barrier seems to be a lack of understanding of the requirement for the provider’s time to perform these visits. The above grid demonstrates that the time requirement for providers is typically no more than 15 minutes per visit yet the reimbursement and wRVUs are considerably greater than that of a more complex follow-up evaluation and management office visit. To achieve 60% penetration of eligible Medicare patients, a provider needs to see only 2-3 patients per day. At this rate of Medicare Wellness visits, a primary care physician can generate additional revenue between $53,000 – $70,000 annually. The revenue for these services is excellent but there is more! Most commercial payers offer incentives for closing care gaps, which is achieved through the health risk assessment where the need for preventive services is identified.
Another program that supports the transition from volume to value is the Transitions of Care program, which is designed to create value by improving outcomes for the transition of a patient from an acute care setting back to home. This program requires an effective communication plan between the inpatient care staff and the ambulatory care staff. There are specific requirements for contacting a patient within 3 business days of discharge to work through transition issues, e.g., medication reconciliation. Medication problems are actually the most common cause for patient readmission to the hospital. A face to face follow-up visit with the patient’s primary care physician is required within 7 days of discharge. One additional interaction with the patient is required between 7 – 30 days after discharge. Then, a claim can be submitted with the specific transitions of care codes. Success in the area of transitions of care is manageable through effective process/change management. The Medicare reimbursement for these services is $165.54 or $232.31 depending upon the medical complexity of the patient’s diagnoses. Commercial payers likely reimburse transitions of care at a higher rate than Medicare. Similar to the Medicare Wellness program, successful transition of care is a service that is largely achieved by the clinical support staff. The provider’s time requirement is similar to a typical extended office visit, i.e., 20-30 minutes.
In our experience, both of these programs, when successfully implemented, create improved job satisfaction of the clinical support staff because they are doing what they were trained to do and working closer to the top of their professional licenses. The physicians are typically happy when their support staff is happy and the entire team is engaged in creating wellness for their patients through identification of previously undiagnosed conditions or confirmation of continued good health. Most importantly, the patients achieve improved outcomes and are more satisfied with their care. The implementation of each of these programs creates the foundation for team-based care, which is critical for success in the value based payment environment.
In today’s reimbursement environment, medical practices can continue to enjoy the same reimbursement for volume that they have always received while implementing the financial and incremental operational transition to pay for value through the Medicare Wellness and Transitions of Care programs.
Innovative Healthcare Teams has had success implementing both the Medicare Wellness and Transitions of Care programs. In the first 6 months after implementation, we saw a volume increase of 178% in Medicare Wellness and over 2,000% in Transitions of Care. This generated an increase of $535,000 of revenue for the health system owned ambulatory practices. It also prevented hospital payment denials for avoidable readmissions as well as penalties associated with the Hospital Readmissions Reduction Program.
Michelle J. Burris, MBA, CMPE is co-founder and Executive Vice President/Chief Business Officer of Innovative Healthcare Teams, responsible for the oversight of all accounting, financial and non-clinical operations for the organization. In addition to her financial and operational responsibilities, Michelle manages the development and marketing of healthcare change management initiatives to assist all clients to achieve their organizational goal of improved patient outcomes and financial performance.
Prior to founding Innovative Healthcare Teams, Michelle held a variety of high-profile leadership positions in the health care industry, including CFO/VP of Operations at Reading Health Physician Network and CFO at both Heritage Medical Group and Lancaster General Medical Group. She began her 18-year health care career with Meridian Health Resources where she held the role of Controller. Ms. Burris has a marked proficiency in the healthcare industry as a skilled financial and operational expert.
The views, opinions and positions expressed within these guest posts are those of the author alone and do not represent those of Becker’s Hospital Review/Becker’s Healthcare. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them.