
The Challenge: Operating Efficiently in a Demanding Healthcare Landscape
The demands for provider pay continue to rise, and healthcare organizations are under mounting pressure to reduce operating costs. Seeking a delicate balance between cost reduction and maintaining the highest standards of care delivery for their patient communities, care institutions should closely examine billing processes for telehealth and locum tenens clinicians in order to stop leaving money on the table.
The Extent of the Efficiency Problem
Despite being renowned for its innovation and advancements, the U.S. healthcare as an industry exhibits tremendous opportunity to increase efficiency across the board. Inefficient processes across the revenue cycle collectively cost healthcare practices billions of dollars each year. According to MGMA, the industry could have saved a staggering $16.3 billion in 2020 alone, representing 42% of the $39 billion spent on administrative transactions tracked by the 2020 CAQH Index.
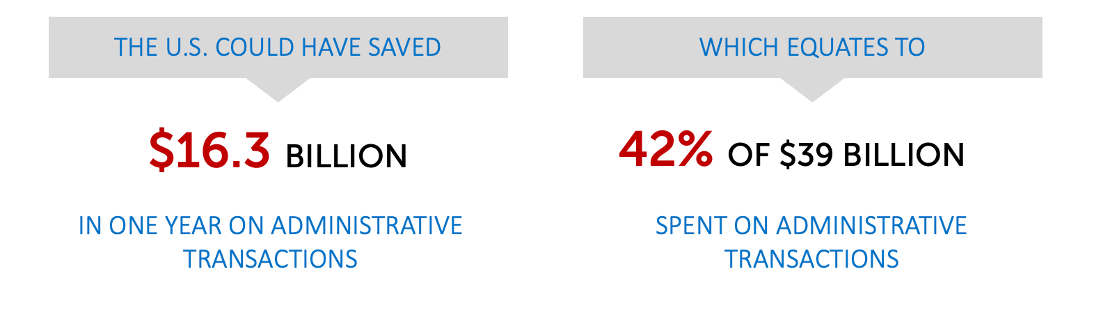
Source: MGMA, How much revenue is your healthcare practice losing due to inefficient revenue cycle processes?
Furthermore, the United States consistently ranks high in healthcare expenditure while lagging behind in terms of health outcomes compared to other developed nations.
A Winning Combination: Telehealth and Locum Tenens
 Telehealth and locum tenens clinicians present two compelling workforce strategies that address the stated demands of healthcare providers. Telehealth offers enhanced patient access, reduced travel time, and greater flexibility in healthcare delivery. Simultaneously, locum tenens clinicians provide valuable support during staff shortages or leave, ensuring continuity of care. The combination of the two has proven effective in restoring and maintaining care.
Telehealth and locum tenens clinicians present two compelling workforce strategies that address the stated demands of healthcare providers. Telehealth offers enhanced patient access, reduced travel time, and greater flexibility in healthcare delivery. Simultaneously, locum tenens clinicians provide valuable support during staff shortages or leave, ensuring continuity of care. The combination of the two has proven effective in restoring and maintaining care.
However, the success of these strategies hinges on correct billing, which is often a complex and intricate process. Healthcare organizations, in their quest for efficiency, sometimes leave money on the table by neglecting to optimize their billing practices.
The Need: Detailed and Ongoing Stewardship over Billing and Enrollment
Creating effective workforce strategies for our clients has revealed the intricate and challenging nature of billing for telehealth and locum tenens services. The process involves numerous intricate details, billing methodologies, codes, and specific parameters that can significantly impact the success of a program based on their precise implementation. Healthcare organizations that collaborate with us gain a valuable advantage through our strategic guidance and support in navigating this complex terrain.
At this year’s National Provider Enrollment Forum, I shared an in-depth walkthrough of locum tenens billing, which presents a fork in the road: the Q6 modifier for services when a physician is away and a locum tenens clinician steps in (which has a 60-day limit), or full enrollment of the locum tenens provider in your group, allowing direct billing under their NPI, with no time limits. For telehealth programs, the Q6 modifier is often unavailable.
Building a telemedicine program also warrants extensive knowledge of billing in order to get the most out of telehealth services. When enrolling telehealth providers, ensure correct organization linkage. Understand distant and originating site distinctions and clarify payor guidelines. When billing for telehealth, adhere to these best practices: include appropriate modifiers (e.g., 95 & GT), use correct place of service codes (02 or 10), and ensure the CPT code aligns with payor regulations to avoid claim denials and delays.
The Strategic Partner Solution
To harness the full potential of telehealth and locum tenens clinicians as strategic solutions, healthcare organizations should consider partnering with experts in the field. Partners like LocumTenens.com possess in-depth knowledge of the billing intricacies that make or break these programs. This collaboration can:
- Maximize Revenue: Comprehensive and accurate billing prevents revenue leakage, ensuring that compensation for services does not go overlooked.
- Speed Up Billing: Partnering with billing experts mitigates time-consuming delays introduced in thorny approval process.
- Streamline Operations: Efficient billing processes reduce administrative burdens, freeing up resources for core patient care activities.
Conclusion: Execution of Billing and Enrollment
The performance of a telehealth program hinges on meticulous management of provider enrollment and billing processes. Overlooking the critical steps within the billing and enrollment processes around telehealth and locum tenens can lead to missed revenue opportunities that compound over time. When it comes to billing for locum tenens providers in telehealth, understanding enrollment options and maintaining best practices are essential steps toward ensuring financial sustainability and operational efficiency. By mastering these aspects internally or partnering with experts, healthcare organizations can set themselves up for long-term success in a healthcare landscape that is evolving rapidly.
