The ramifications of this decision extend well beyond the impact on consumers covered by United or to the competitive imbalance the departure will create in a number of markets. Hospitals with patients on a United exchange plan must now figure out how to fill a new hole in their revenue model.
Whenever I talk about today’s managed care function with hospital execs, I can’t emphasize enough the importance of modelling out ‘what if’ scenarios. Whether it’s a decision such as the one United has made, consolidation among payors or large employers moving from one payor to another there’s simply too much at stake to be caught off guard.
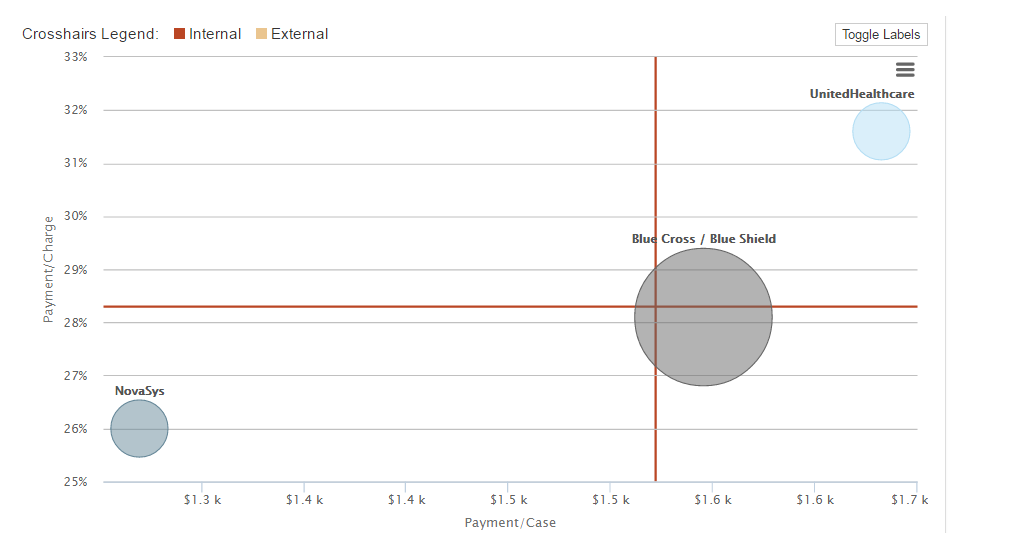
Take a look at the image below from our INCONTROL solution. In this case, United is paying more than 31 percent of charges. If those Exchange patients were to switch to NovaSys, for instance, payment as a percentage of charges would drop from 31 percent to 26 percent. So in other words, about one-sixth of the revenue for those patients would vanish.
For hospitals with patients utilizing a United exchange, you should be exploring the potential impact sooner rather than later. Consider these questions:
• If patients currently with United move to another exchange plan, what will be the impact (positive or negative) to revenue?
o In a state such as Arkansas where the only other choice in some counties is BCBS, what would revenue for your United volume look like at BCBS rates?
• What happens if those United patients (all or a sizable portion) opt to become uninsured and pay out of pocket for services?
o Can you shoulder a potential increase in bad debt?
o Are your charges on par with the rest of your market or might patients be compelled to shop around?
Today hospitals must have a good understanding of all aspects of patient revenue and be able to explore – proactively – various ‘what if’ scenarios. Not only do you gain insight into potentially troublesome scenarios but you gain access to a deeper, more holistic lens into your payor relationships. This perspective is critical in developing more collaborative, mutually-beneficial relationships with key payors.
The views, opinions and positions expressed within these guest posts are those of the author alone and do not represent those of Becker’s Hospital Review/Becker’s Healthcare. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them.
