Implications for providers engaging in new payment models
This content is sponsored by DataGen.
Variation in healthcare spending across the country and, in some cases, within the same markets, has been the subject of debate for decades. Now, as bundled or episodic payments have come under the microscope as a payment model with potential to improve outcomes while reducing costs, payment variation within and across episodes have come into sharper focus. What drives the variation in payments when providers are caring for similar patients? Is it the hospital stay? Post-acute care? Practice patterns? Payer issues? And, more importantly, what does this mean for hospitals and health systems considering assuming risk under bundled payments?
This Executive Briefing seeks to answer some of these questions by exploring the regional variations in Medicare payments for 90-day episodes of care (those beginning with a hospitalization that also includes post-acute care). It provides key findings from an analysis conducted by DataGen on four different clinical episodes/areas of care: acute myocardial infarction, congestive heart failure, pneumonia and major hip and knee joint replacements. These four areas represent some of the highest volumes of inpatient care within the Medicare population and are areas where CMS is focusing much of its measurement and quality-related payment policies.
Using calendar year 2012 data from the 100-percent Medicare Standard Analytic Files and applying the definitions currently used by the Medicare Bundled Payments for Care Improvement program, episodes in each of the four clinical areas were reviewed. Under BPCI, episodes are defined by the initial inpatient stay and are assigned to Diagnosis Related Groups. The DataGen study examined the entire family of DRGs for each condition (e.g., for AMI, the episode family includes DRGs 280, 281, and 282). The impacts of Medicare "add-ons" that can cause variation in payments that are not related to the provision of care were removed, including area wage adjustments, payments for medical education and disproportionate share, and capital. This step, which is often missing from other studies of variation, was taken to neutralize or standardize payments to enable fair comparisons between regions.
Some of the key findings from DataGen's analysis affirm other published studies on the drivers of payment variation, but other factors also emerged. These findings may have implications for future payment policy, as well as for hospitals, health systems and other providers considering participation in risk-sharing initiatives such as bundled payments.
Key findings
To explore variation in episode payments, DataGen identified the 10 most and least expensive regions in the country for each episode type. Differences in Medicare payments were quantified between the highest and lowest regions, with the goal being to determine the reasons for those differences.
Overall, our analysis revealed:
- Variation is not driven by the initial hospital stay. When looking at episodes of care that are defined by a DRG, the inpatient stay is generally not the driver of cost differentials because those payments are standardized. The variation between episode payments, in three of the four clinical areas, was driven primarily by post-acute care choices and utilization. This finding affirms other studies about variation across Medicare episodes of care.
- For CHF, readmissions and skilled nursing care were the main causes of payment variation. An episode of care for patients admitted to the hospital and diagnosed with CHF costs the Medicare program an average of $21,660 in the most expensive 10 regions and about $17,130 in the least expensive 10 regions — a 26 percent difference.
- In the 10 lowest cost regions, almost half of the CHF episodes did not utilize any institutional post-acute care, lowering the average payment for those episodes to $10,000.
- Correspondingly, the 10 most expensive regions did not utilize any institutional post-acute care for about 30 percent of their CHF episodes.
- The readmission rate for CHF is 40 percent in the lowest cost regions and 51 percent in the highest-cost regions.
- For pneumonia, payment differences are due primarily to readmission, skilled nursing facility and long-term cost hospital post-acute stays. The Medicare program paid an average of $20,750 for pneumonia care in the 10 most expensive regions and an average of $15,280 in the 10 least expensive regions, a difference of 36 percent.
- For major joint replacements (hips and knees), the principal driver for payment differentials was post-acute rehabilitation utilization. The DataGen research team expected to find less payment variation between regions for the major joint episodes based on the assumption that care patterns for a surgical procedure are more clearly defined than for medical conditions. However, the findings showed a difference of 27 percent between the average episode payment in the most expensive and least expensive regions — about $28,290 per episode vs. $22,290. The predominant cause of this variation was among the post-acute rehabilitation settings — inpatient rehabilitation facility, SNF and home health care — with the 10 most expensive regions reporting significantly higher costs in all three rehabilitation settings.
Perhaps the most dramatic finding — with potential implications for care redesign and bundled payments — was among the AMI episodes. While much of the variation in patient-centered episodes of care for CHF, pneumonia, and major joint replacements is driven by readmissions and post-acute care utilization, the DataGen analysis shows a major driver of the variation in payments for AMI DRG episodes is the volume of direct transfers from the initial hospital to another acute-care hospital. In the highest-cost regions, about half of all the acute care transfers for AMI patients were for percutaneous coronary intervention, also known as angioplasty, and possible stent placement.
The AMI episode conundrum
A patient who experiences a heart attack (AMI) and is admitted to the hospital may be assigned to one of several DRGs depending upon the care that person receives during his or her inpatient stay. In the instance where a patient is diagnosed with an AMI and then requires a PCI, the patient will be either:
- Admitted to the hospital with an AMI and receive the PCI procedure at that hospital. In this case, the first and only DRG assignment will be PCI, not AMI; or
- Admitted to the hospital with an AMI, and then transferred to another hospital for the PCI. This results in two DRG assignments: one for the AMI treated at the first hospital and one for the PCI performed at the second, transfer hospital.
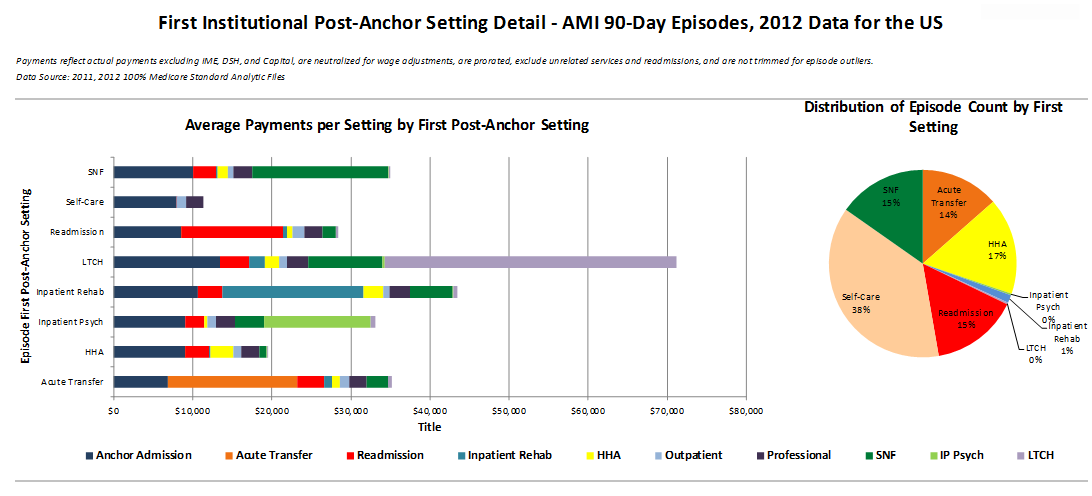
When reviewing only those episodes of care that began with a DRG assignment of AMI, of the more than 41,000 qualifying Medicare episodes across the country in 2012, 14 percent were transferred to another acute-care facility and 5 percent had a PCI at the transfer hospital. Nationally, Medicare payments (i.e., costs to the program) for AMI acute care transfers (not just those receiving PCI) were second only to the costs for patients going to long-term care (Figure 1). Figure 1 shows the average cost of care for episodes stratified by the first institutional setting that a patient goes to after discharge. The costs to the Medicare program for all settings both before and after the first institutional setting are represented by different colors. Figure 1 also shows the percentage of episodes in each category of the first institutional setting.
Figure 1
Looking at the most expensive region in the DataGen study, acute-care transfers of patients in an AMI DRG occurred 36 percent of the time and, among those transfers, almost half received a PCI at the second hospital; that is, 17.5 percent of the AMI episodes in the most expensive region were transferred for a PCI (Figure 2). For those episodes, the average length of stay for the initial inpatient stay was just under three days — these were not one-day stays where the patient was stabilized and immediately transferred out.
Figure 2
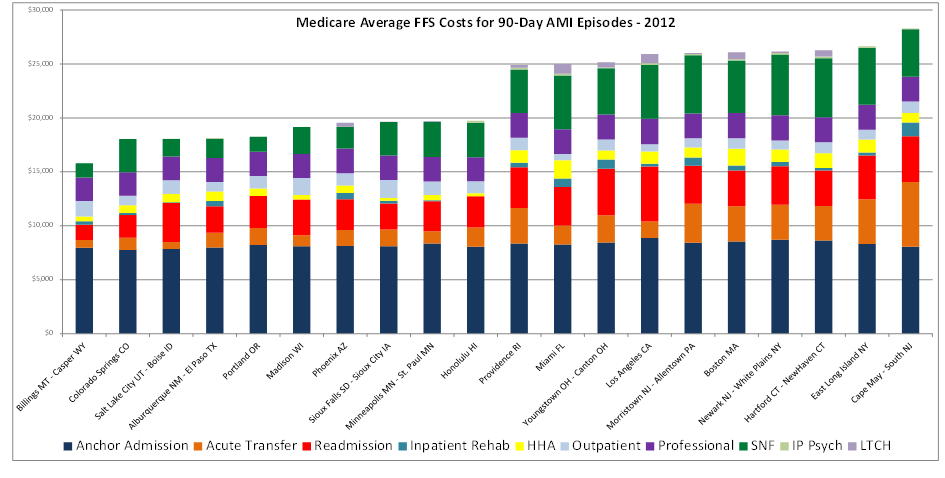
Upon identifying that patient transfers for PCIs were driving significant payment variation, the DataGen research team initially assumed that inpatient PCIs were more commonly performed in the most expensive region than in the least expensive region. Further analysis revealed that the opposite is actually true. Sixty-five percent of the episodes with a principal diagnosis of AMI in the least expensive region, Billings/Casper, received an inpatient PCI, either during the initial stay or in a subsequent admission; in the most expensive region, Cape May, that percentage is 44 percent.
Next, DataGen examined whether transfers were more likely from hospitals that do not perform PCIs. Surprisingly, the data indicate that in numerous instances, hospitals with the capability to perform PCIs are still transferring some of their heart attack patients to other hospitals. Finally, these same regions with higher volumes of transfers also see significantly higher payments for readmissions, SNF and home health care — the subsequent interventions are not saving enough costs downstream to offset the additional upfront costs.
Opportunities for efficiency in treating AMI Patients
When looking to redesign patient care for improved outcomes, cost-effectiveness and efficiency, the intent is to provide services to and payment for patient-centered care. Looking at the AMI episodes of care, there are clear opportunities to reduce costs by ensuring that patients are treated in the most appropriate setting.
There are three scenarios for care based on the AMI findings:
- In hospitals that are licensed to perform PCIs, a patient who is admitted with AMI and needs a PCI receives his or her full treatment at that hospital. This results in one DRG assignment and payment for the PCI.
- In hospitals not licensed to perform PCIs, a patient admitted with an AMI who needs a PCI will be designated as an AMI DRG at the first hospital and then be transferred to another hospital for the PCI. This results in two DRG payments, one for the AMI care and one for the PCI. In this case, the inpatient acute care costs of the patient’s episode of care are doubled.
- In hospitals that are licensed to perform PCIs, a patient who is admitted with an AMI and needs a PCI receives some care at the first hospital and then is transferred to another hospital for the PCI. This also results in two DRG payments and twice the inpatient acute-care cost.
The first scenario would appear to be the preferred care pattern and it is very common. However, patients experiencing symptoms of a heart attack may present at any hospital emergency room. It is not always apparent upon patient intake that the diagnosis will be an AMI and that the treatment will require a PCI — that is why the second scenario is also common. The question in those instances is whether full payment for that first inpatient stay is appropriate, given that the patient is receiving further care for the same heart attack at another hospital. The long LOS data for these cases may indicate that services and care are needed to stabilize the patient, or it might indicate the need to wait until the transfer hospital can schedule the PCI. The administrative data do not provide enough detail to fully examine the medical efficacy of a complete AMI inpatient payment when it is followed by a PCI inpatient stay; this requires further studies and interviews for more definitive commentary.
The area with the most opportunity for care redesign and program savings is the third patient care scenario — hospitals that are licensed to perform PCIs but transfer a patient to another facility for the procedure. It would appear that in these instances, either the patient is choosing to receive the intervention at another hospital, perhaps a specialty hospital, or the initial hospital does not have a full-time interventional cardiology program. This too requires further study about why these transfers occur — for example, whether they are being performed after hours or on weekends — but the potential is evident and could have significant implications for public health policy related to part-time surgical coverage.
Implications and considerations for providers accepting risk
There are a number of important lessons to be learned from this targeted and limited data review:
- Providers need to look at and use data in a new way. Care redesign and true program savings can only be accomplished when the entire episode of care is examined — not just the inpatient hospital cost — and patients are at the center of that care. Whether it is bundled payments, accountable care, medical homes or any other risk-sharing arrangement, the emphasis is always on managing the whole episode.
- Hospitals should be cautious about engaging in episode payments for diagnoses, such as AMI, which may require a procedure not performed on a full-time basis within the hospital or for which specialty hospitals are in close proximity. In the case of AMIs and PCIs, hospitals that do not perform this procedure, or do not have a full-time interventional cardiology program, are at a disadvantage when it comes to clinically and cost-effectively managing care.
- It is essential that providers accepting risk through new payment models identify the most clinically appropriate and cost-effective settings for post-acute care. This requires an examination and comparison of outcomes (e.g., readmissions) and costs of the post-acute care options available, and then communicating those findings to physicians and other clinicians who are accountable for managing patient care.
