Some healthcare organizations are using a new best practice called time-driven, activity-based costing1 to help maximize their EMRs. TDABC records the consumption of resources by activities or processes to determine how costs are allocated throughout the entire hospital system. Implementing a TDABC solution not only leverages EMR investments but also provides insight into where you are making and losing money. It delivers an accurate view of the economics of your system’s operations. TDABC allows hospital systems to apply cost to the entire patient encounter, regardless of the location of services.
The current state of healthcare environments and economics
According to a new study from the University of Michigan School of Public Health, physicians who have made the switch to EMRs and don’t maximize their ability to enhance revenue and cut costs have a significant chance of losing tens of thousands of dollars over five years. Even more critically, the study revealed only 27 percent of providers showed a positive return on their investments.
Without a reliable and accurate cost accounting system, hospitals and health systems cannot prepare for the myriad of changes (end of fee-for-service, risk-based or shared reimbursements, etc.), nor can they accurately measure costs and compare them with outcomes.
The limitations of the current decision-support systems
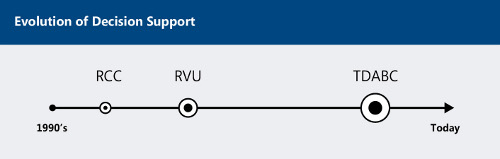
The majority of today’s hospital systems depend on outdated, imprecise decision-support systems that rely on either ratio-of-cost-to-charges or relative value unit costing. These systems have worked sufficiently well until now, but the limitations will soon become very apparent as the Patient Protection and Affordable Care Act requires healthcare providers to participate in shared or “bundled” reimbursements among multiple parties. Both methods are simply “peanut-butter spreading” the costs to monthly charges and do not reflect variation in patient care.
Ratio-of-cost-to-charges
RCC is a method used by a large number of hospital systems, wherein costs are allocated on a patient-by-patient basis then converted to costs using their specific RCC. For example, according to the American Hospital Directory, if a patient had $300 in pharmacy charges, and the hospital’s RCC for pharmacy was 0.5, then the cost would be allocated as $150. But RCCs are an imperfect science because assigning costs to patients based on what hospitals charge can often be misleading.
Relative value unit
RVU is a measure of value used by hospitals to compare the amount of resources required to perform various services within a single department. RVUs capture the relative level of time, skill, training and intensity needed to provide a given service. RVU costing relies entirely on the current fee-for-service reimbursement environment. Once this form of reimbursement diminishes, so will the remaining value of these outdated decision-support systems.
Figure 1.
Time-driven, activity-based costing: The next generation in decision-support systems
In a healthcare market focused on change, it is critical to manage costs and make the most of EMR investments. By applying time-driven activity-based costing, hospitals can quickly determine how the cost of different approaches impacts outcomes, ultimately providing a more positive influence over profitability.
Here’s how it works.
Establishing accurate estimates: TDABC accurately estimates cost and demand by measuring the unit cost of supplying capacity and the time required to perform a transaction or an activity.
Tying patient transactions to resources: For hospitals, TDABC leverages patient transaction details from patient charting, CPOE and other modules of the EMR to appropriately align resources and cost to each patient visit.
Tracking procedural, time and effort for each procedure: The data tracks a variety of discrete tasks and events. In addition to tracking chargeable procedural information, it also tracks details that can indicate patient acuity and the level of effort required from nursing and other areas without event-specific charge codes.
This allows hospitals to make complete operational use of the EMR data, elevating the EMR to more than simply a data-gathering and reporting tool primarily used for coding and billing accurately. Combining the event details tracked in the EMR with clinician-provided estimates of effort allows the hospital to evaluate capacity utilization across all clinical, clinical ancillary and non-clinical departments to identify staffing needs and align potential budget and cost saving discussions with the true impact on patient care and services offered.
Figure 2.
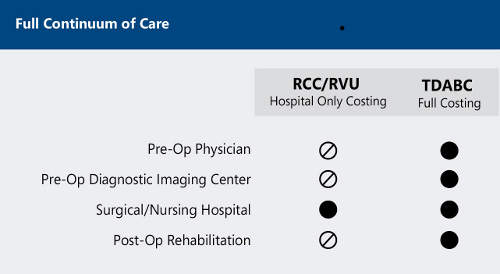
Figure 3. Comparison of the RCC, RVU and TDABC cost accounting systems

Making the most of your EMR
Hospitals should use TDABC to record the true consumption of resources, which allows them to gauge this against the expense recorded in the monthly GL and to manage their utilization of resources. Current EMR systems are unable to complete this type of analysis given their design point on charges.
Using TDABC, hospitals can achieve a greater return on EMR investments. By leveraging the wealth of transactional detail in EMRs and applying cost to these transactions, health systems can finally derive the true and actual patient care costs. Clinicians and care providers will see the value derived from accurately documenting patient care and will understand the importance the EMR brings to their department or area of the hospital.
Figure 4.

1. Kaplan, R. S. & Porter, M. E. (2011, September). The Big Idea: How to Solve the Cost Crisis in Health Care. Harvard Business Review, 3.
More Articles on Electronic Medical Records:
Electronic Health Records: The Good, the Bad and the Ugly
4,000 Clicks Per Shift: ED Physicians’ EMR Burden
What Physicians Like and Dislike About EHRs
