Further, in a post-pandemic study, more than 30% of nurses reported concerns about their emotional health, citing insufficient staffing levels and its impact on their health and well-being as the main reasons for leaving the profession.
These overlapping trends are resulting in health systems losing more than 2 million years of combined nursing experience each year.
At Becker’s 11th Annual CEO + CFO Roundtable, in a session sponsored by Trusted Health, two leaders from Mercy (St. Louis) — Cheryl Matejka, CFO, and Betty Jo Rocchio, DNP, senior vice president and system chief nursing officer — discussed how the right workforce management platform can help organizations redesign their staffing models in tune with nurses’ evolving needs, while saving costs and improving operational efficiency.
In Mercy’s presentation to over roughly 100 hospital executives there were three major themes.
1. In the post-pandemic era, organizations must strive for a multi-generational staffing model redesign
Two phenomena have recently converged: The COVID-19 pandemic and generational differences in the importance that people place on their jobs. As a result, there’s a far greater emphasis on work-life balance and flexible compensation today. These preferences are more pronounced in generations Y and Z (“millennials” and “Zoomers”) than in generation X and baby boomers, but these trends are increasingly cross-cutting.
“What we saw during the pandemic was that nurses left us for increased compensation — but compensation wasn’t the main driver,” Dr. Rocchio said. “Their workload for what we were paying them was the main driver. We’re noticing people are no longer tolerating what happened to them before the pandemic.” She noted that in addition to a more balanced workload, nurses want more control over their schedules.
Despite these accelerating trends, many organizations’ workforce management cultures are stuck in traditionalist thinking that reflects inflexible ways of working. Changing that requires a bold new vision for redesigning the nurse staffing model.
2. Successfully redesigning the staffing model requires transforming 4 key elements
There are four factors that determine the success and sustainability of healthcare organizations’ workforce strategies. To bring their strategies in line with evolving worker expectations, which positively impacts vacancy fill rates and nurse satisfaction, hospitals and health systems need to redesign staffing by focusing on:
- Maximizing flexibility by maintaining local and regional float pools of nurses credentialed to work in specific hospital units, as well as a pool of credentialed “gig” nurses. This layer of flexible workers supplements the organization’s core layer of full- and part-time nurses and its agency layer of external and international nurses. “This middle layer is the secret sauce and has to be designed with great precision and definitions,” Dr. Rocchio said.
- Giving more choice and control over schedules and compensation by using Works technology. In automating the scheduling system across all units, equipping it with automated nurse credentialing, making it accessible to the entire available labor pool via a user-friendly platform/app and providing information about how each shift is compensated, hospitals can ensure units are safely staffed while giving nurses autonomy over when they work.
- Broadening access for multiple workforce layers and generations. At Mercy, core staff members have priority access to and right of first refusal for available shifts, which then become available to the flex workforce. “During the recruitment phase, we tell job candidates: ‘If you need benefits, you’re going into the core layer. If you want maximum flexibility and don’t need benefits, you can go into either the local float pool, the regional float pool or the gig layer,’” Dr. Rocchio said. “That allows them to choose where they want to work.”
- Enabling scalable technology integration with automation and artificial intelligence that pinpoints where the greatest needs are. “Before we had a technology-driven system, we were offering incentives for shifts based on whatever nurse managers thought they needed,” Dr. Rocchio said. “Today, it’s completely automated and we are using incentives to fill our hardest-to-fill shifts.”
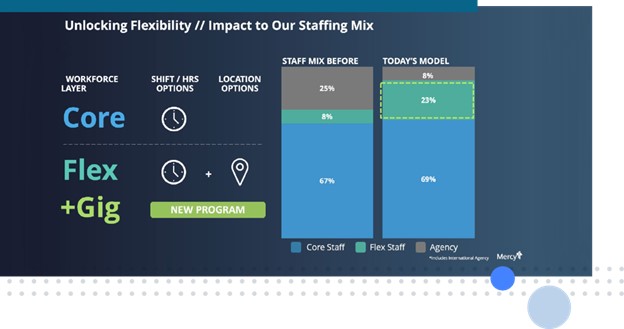
After partnering with Trusted Health and implementing their Works platform, Mercy saw significant changes to its staffing mix, which improved flexibility and workload for workers while reducing agency spend for the organization. Before the partnership, Mercy’s staff mix comprised 67% core staff, 8% flexible staff (including local and regional float pools) and 25% agency staff. After the partnership, the mix became 69% core, 23% flex/gig and only 8% agency staff.
Amid persistent staffing challenges, such shifts to the staffing mix are important because they can impact the rate at which organizations fill open shifts. When shifts cannot be filled with flexible or agency staff, the excess care burden falls on core staff; thus, one of the main benefits of increasing flex staff is to lighten the workload on permanent workers and reduce burnout and attrition.
Yet, while flex staff serve a similar function to agency staff, they are less costly and generally have higher levels of commitment and familiarity with the organizations that credential them and that they repeatedly work with. “While we will always need some of the agency layer, we want to minimize that so we have nurses who are most familiar with our care model and our system works more consistently,” Ms. Matejka said.
3. Increasing flexibility and autonomy in staffing translates to cost, time + FTE savings
In fiscal year 2023, after transitioning to Trusted Health’s platform for recruiting a flexible workforce of nurses and allied health professionals, Mercy realized $30.7 million worth of savings associated with rate reductions in premium labor spend. Those savings were due to a decreased reliance on agency staff because of the availability of an alternative flexible workforce (float pools and gig workers) that became more easily discoverable through the platform. In turn, that led to a 62% reduction in agency spend and a 16% reduction in total care costs as a result of optimizing the nursing workforce.
“There are a lot of workforce platforms out there, but what you should really demand is automation, such that no one is ‘touching’ things — begging staff members to come to work or trying to get them paid,” Ms. Rocchio said. “It should be an automatic flow through your systems.”
At a more strategic level, automation can also act as a form of governance by ensuring fairness and transparency in pay across health systems. “If you have multiple locations, you’re going to have multiple opinions on what you should be paying per shift,” Ms. Matejka said. “Automation ensures that we don’t have rogue units that are going off and paying crazy amounts per hour.”
In addition to savings linked to pay efficiency and transparency, Mercy’s adoption of Trusted Health’s technology has also led to:
- 20% less time spent on staffing and scheduling tasks
- An increase in the organization’s fill rate from 83% to 86%
- A total of 102 equivalent FTEs saved, even as bedside FTEs increased by 3.5%
- 8% reduction in turnover, including a 9% reduction in first-year turnover
- 4% reduction in vacancy rates
“It’s an overall pretty successful effort, but it requires continuous monitoring and tweaking to sustain,” Ms. Matejka said. “We can’t let our foot off the pedal as we work to hardwire the thinking.”

This Playbook will be presented at Becker’s Annual Conference live session on April 8th with Betty Jo Rocchio, join her Featured Session.
