There are three critical components to implementing a bundled payment program.
Across the healthcare market, many organizations are implementing bundled payment programs as they execute their value-based reimbursement strategies. The development of these programs has typically been driven by the demand from leadership to implement operational improvements, offer core service differentiation, and meet patient demand, as well as seek tighter physician alignment and additional incremental volume. When it comes to developing a bundled payment program, it is optimal to proceed through the following three phases: making the decision to offer a bundle, selecting the appropriate bundled program, and implementing the program. The insights shared here apply to organizations that are addressing the challenges of successfully implementing a bundle. Providers that have not yet made the decision to pursue a bundled payment program or selected which services to bundle should review Articles 1 and 2 in this series.
Putting the plan in action
Implementing a bundled payment program involves participation from and coordination among the physicians, hospital, and payor. Each of these stakeholders has a critical role to play. As the providers of care, physicians should be heavily engaged to ensure buy-in. The hospital needs to make sure that its operations, both clinical and financial, are effective and efficient. Payors need to partner with hospitals and physician groups to create attractive financial incentives for program participants. Let's dive deeper into these components and the importance of each in implementing a bundled payment program.
Physician engagement
Active and consistent physician engagement is the first major component of a successful bundle. A value-based arrangement is a departure from the norm for physicians, even those who are employed by large health systems. It is common for physicians to be skeptical about the implications of or need for a bundled payment program or be very resistant to placing any amount of reimbursement at risk. However, they understand where clinical and process improvement opportunities exist, and therefore to achieve success, physician engagement and consensus are essential. Physician leadership can take several forms:
» Participating in the general development process, including the agreement terms
» Identifying and driving the clinical protocol changes for patient care
» Encouraging colleagues to reduce unwarranted variation
» Crafting the services to be included and managed in the bundle
Ensuring physician engagement can be a long and incremental process over the course of several months, depending on the history of the interactions between the hospital and physician entities in the market. Achieving physician engagement requires that the planning group clearly demonstrate for physicians the value and impact to patients and providers, as well as be transparent with updates and proposed terms. Physician participation also requires the creation of financial incentives, typically in the form of a shared savings distribution or quality performance payments from an incentive pool. Many health systems provide physicians with a stipend for the time they dedicate to the program's development. Note that both payment for physician time and reimbursement under the bundled payment program are a sensitive fair market value issue. Some of these concerns can be mitigated if the bundle is exclusively for commercial patients; however, legal counsel should be involved to ensure payments fall within FMV. The structure of the shared savings payments are discussed below in the "Payor partnership" subsection.
Operational readiness
A successful bundle relies on the execution of key tasks both along the continuum of care and according to the financial funds flow. The responsibility for these tasks is usually assigned to hospital staff. A hospital's ability to smoothly process and track patients in the bundle and follow the financial funds flow is important for avoiding fiscally negative outcomes and cost overruns. Often, organiza-tions are not prepared for the challenge of tracking a bundled population and are not familiar with the constant diligence required to minimize unwarranted variation and costs.
The bundled programs that run the smoothest exhibit a high level of transparency and consistently share reliable data among the providers, including the hospital and physicians. This is important for two reasons: (1) to ensure consistency and high-quality patient care and (2) to avoid questions regarding the validity of the program's finances. A key step in the development process is to conduct a readiness assessment that evaluates the organization's ability to pay under a bundled contract, as well as monitor and track reimbursement. Often, the assessment identifies required changes that include:
» The development of an accounting and funds flow process to track and adjudicate the reim-bursement under a bundle.
» Technology system updates (EMR, finance).
» Staff education on clinical protocols.
» Patient education regarding bundled clinical protocols.
» Revisions to patient care plans (e.g., post-acute) for the appropriate level of care.
» Program marketing to providers and patients.
Conducting an assessment and establishing the organizational capabilities to process a bundle can take several months, depending on the required changes. Achieving a ready state at most hospitals involves identifying key personnel along the care continuum to be responsible for tracking the patients, putting in place processes to support tracking, and dedicating resources to make any required technical or work flow changes. During the term of the bundled contract, the regular reporting of outcomes and other clinical information to a work group of physicians and hospital administration will be important to maintain supervision and control. Demonstrating this operational readiness is the second critical component.
Payor partnership
The final phase required for a bundled payment program is the partnership with the payor, which can be a self-insured employer, commercial health plan, or government payor. Arrangements with government payors are prestructured, but those with commercial payors have much more flexibility. The commercial payor partner will be seeking more financial cost certainty associated with the offered bundled and will want to demonstrate value and quality to its customers. The most successful bundles are those that have a payor partner that is willing to engage in a discussion, offer insights and suggestions regarding post-acute care networks, and share in the effort to craft a bundled offering that is attractive to the market.
The partnership comes together in the bundled payment agreement. The bundled payment contract will include several elements, including the specific scope of service (i.e., included and excluded procedures, service quality levels, ancillaries, post-acute providers), the financial terms (e.g., risk corridor, volume guarantees, performance or quality incentives), and the proposed payment model and funds flow (e.g., prospective versus retrospective, physician participants, hospital participants, post-acute care participants).
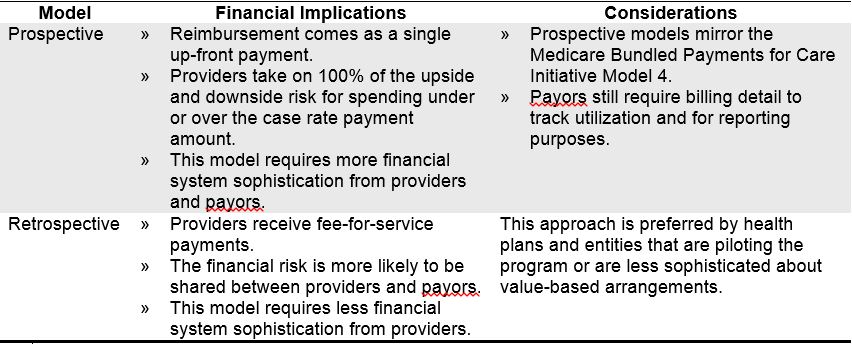
The contract term that is often the most challenging to agree upon, and explain, is the payment model approach—the retrospective model versus the prospective model. An overview of the attributes of each model is provided below.
Bundles are often established as separate contracts with the payor, but can also function as addenda to existing contracts. Separate agreements are usually associated with a prospective payment model, and addenda are more commonly correlated with a retrospective model; however, either contracting approach is applicable to the two payment models.
In addition to the payment model, the actual funds flow among the providers is a common topic for discussion. Payments derived from savings are typically shared in a meaningful way with physicians. The distribution of shared savings among physicians is also a key point of discussion, as the payment amounts between specialties (e.g., orthopedics, cardiology, and anesthesia for a joint replacement bundle) must be agreed upon. Regardless of the final distribution of funds, establishing a willing payor partner to work with on a bundle is the third critical component for a successful bundled payment program.
Ensuring success
Execution of a bundle requires the joint efforts of myriad partners from the hospital (e.g., operations, finance, clinical), physicians, and payor. Careful consideration of and adherence to the plan outlined above, along with the key involvement of critical stakeholders, will ensure that the bundled payment program has operational success and accomplishes its strategic objectives. An organization that has gone through the three development phases (making the decision to offer a bundle, selecting the appropriate bundled program, and implementing the program) will be more assured of making a sound strategic decision and maintaining and building a successful and sustainable program.
Jason Lee is a senior manager with ECG. In more than a decade as a healthcare industry consultant, Jason has worked with health systems nationwide to create hospital/physician alignment structures and optimize innovative reimbursement mechanisms. He is a nationally recognized speaker on managed care and health exchange issues.
Terri Welter is a principal with ECG. She leads ECG's Contracting and Reimbursement practice, where she has assisted dozens of hospitals and medical groups in the financial planning, assessment, and negotiation of their managed care contracts. She has been the featured speaker on managed care and provider reimbursement for a variety of national professional associations.
The views, opinions and positions expressed within these guest posts are those of the author alone and do not represent those of Becker's Hospital Review/Becker's Healthcare. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them.