With larger employers increasingly exploring direct contracts with health systems including ACOs, a body of experience can be drawn upon from Medicare ACOs.
There are currently 561 ACOs with 10.5 million assigned beneficiaries participating in the Medicare Shared Savings Plan (MSSP) (CMS, 2018). Many organizations began participating in a commercial ACO with traditional up-side risk models, bundled payments, or medical homes. A few challenges to be aware of include meeting national quality score averages, working within limited networks, access to multiple data sources, and failing to consider important fiscal targets.
Results for MSSP plan year 2015 showed that 400 ACOs generated $466 million in savings and 31% (125 ACOs) reduced costs and achieved payout thresholds while 21% (81 ACOs) reduced costs but did not meet payment thresholds, according to the Center for Medicare and Medicaid Services. Given the opportunities and challenges, it is key for health systems to understand the elements of high-performing ACOs and use this knowledge to build or improve their commercial offerings for employers.
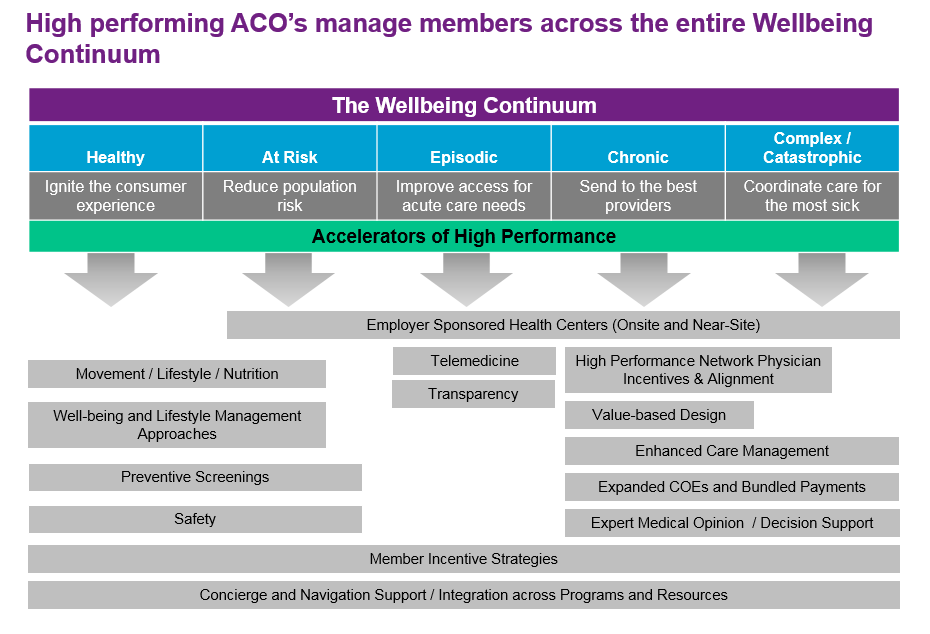
Additionally, health systems should understand the leading priorities of the employer market. Most employers seek to align their benefits with the entire wellbeing continuum for their employee population: from providing preventative screenings to the healthiest patients to efficiently coordinating care for the most sick, as well as providing effective navigation support and consumer-grade patient experience that meets needs across the wellbeing spectrum. High-performing ACOs already manage their members across the entire wellbeing continuum.
For success in the commercial market, health systems should assess five drivers of high-performing ACOs:
1. Governance structure
2. Network
3. Care model
4. Financial model
5. Consumer experience
1) Governance
Health systems should include clinical leaders throughout the organization who are accountable for achieving high performance and driving the organization to continuous improvement. Engaging clinical leaders aligns incentives and improves buy-in translating to greater success.
These clinician leaders should have a level of authority and accountability to set organizational strategy, goals, and tactics in their organization alongside other business leaders. This dual leadership model reinforces the aligned organizational and clinical goals achieved by successful ACOs.
2) Network
An effective ACO must serve member needs across the wellbeing spectrum by including the right mix of clinicians serving members in appropriate settings. This access to a quality delivery network forms the foundation of the ACO. High-performing ACOs have optimized care delivery across primary care physicians, specialty physicians, and hospital-based physicians to ensure the wellbeing continuum is met for all members under the ACO.
3) Care Model
The most difficult challenge for ACOs is defining and implementing care models that address different components of the wellbeing continuum due to the complexity of chronic condition care and the increased number of stakeholders involved, but doing so is key to achieving efficient, effective outcomes with engaged patients.
Care model components that should be assessed are:
• Medical Home: Effective health systems not only have the ability to coordinate care across small groups of members in multi-disciplinary teams, but also optimize their medical homes across all important member groups.
• Target Population: Understanding and managing the target population is required to direct limited resources to the right population, which is especially salient with high-risk conditions and procedures, and transitions of care. High-performing ACOs include all members as part of their targeted approach.
• Clinical Guidelines: The ability to develop, implement, and measure evidence-based guidelines for the most prevalent conditions is critical. Spreading guidelines across the entire organization is seen in high-performing ACOs.
• Quality Metrics: While measuring quality outcomes is an important component of all ACOs, high-performing ACOs incorporate continuous quality improvement methods across the entire ACO. Success is built from rapid cycle learning to quickly identify care processes that work and eliminate those that don’t.
• Care Coordination: Coordination of care has become increasingly important with organizations identifying barriers to effective coordination in existing delivery models. High-performing ACO’s drive care coordination from within the organization and hold their clinicians and staff accountable for breaks in coordination, reducing duplication, waste and unnecessary care.
• Site of Care: Performing the “right” care in the “right” setting is an important area of focus for organizations that look to improve their effectiveness and efficiency with members. High-performing ACOs have fully integrated efficient sites of care for any member condition and hold their clinicians accountable for ensuring care is delivered in these efficient settings.
• Pharmacy Management: Actively managing members’ prescription use across the organization is another way to improve outcomes and efficiency. This includes generic prescribing, poly-pharmacy and medication reconciliation programs. In addition to these common actions, developing evidence-based medication protocols and applying them across all drug categories – oral, injectable, and infusions are seen as addressing potential out of control specialty pharmacy costs facing most employers. High-performing ACOs have value-based programs across all sites and members.
4) Financial Model
As health systems try to bend the cost curve down, cost of care is an important goal for ACOs while managing the above elements of an effective care model.
First, ACO risk should be addressed. Namely, what is the organizational risk and how much control do the clinicians have over that level of risk? Secondly, a firm understanding of how clinician incentives align with goals is needed. Incentive based compensation is an increasingly important part of the move to value-based health care, and accordingly developing robust compensation models that are based on outcomes, service levels and efficient use of resources will become increasingly important for all payer categories.
High-performing ACOs take full risk for their member population across professional and institutional coverage. In addition, they have well established compensation models with all physicians that align performance with incentives in a balanced scorecard approach.
5) Consumer Experience
A critical way for health systems to capture the value created through ACOs is to provide members a thoughtful and seamless experience without roadblocks that could push members toward suboptimal routes in pursuing care. Access, availability, proactive outreach, and web-based content are all important components to drive member satisfaction. High-performing ACOs have consistent and easy access to 24/7 care, and advice and resources through tools that meet member expectations. They develop a concierge approach to member satisfaction and try to meet individual member needs through customization. Ensuring a quality experience enables the desired behavior from patients, supports effective engagement with the system’s care management functions, and provides consumer-grade operational elements like online, same-day appointments.
Leveraging ACO drivers to be competitive in the market
Health systems should assess how they stack up on these five drivers before launching an ACO to understand their strengths and weaknesses. In order to do this, there are a number techniques available to assess what improvements are needed and where opportunities exist. An effective approach includes:
1) An assessment of the market of employers in the area and their needs can help a health system find the right direction. Evaluating the local market should include ensuring there is access to enough potential members to reach a volume that will sustain operations and allow improved care coordination.
2) A review of whether they have a financial management foundation that will support effective risk management and mitigation. The financial model should be complemented by an evaluation of risk mitigation strategies and monitored to ensure the ACO is not carrying excess risk.
3) An analysis of their own experience managing the care of their own employees as a unique way to assess their network and offerings, and understand how to use this knowledge to provide robust services to the employer market.
Contact
Daniel Cusator
+1 714 814 6611
dan.cusator@willistowerswatson.com
Jessica Jones
+1 312 873 5126
Jessica.jones@wilistowerswatson.com
