Broad and widely available interoperability between all providers has been on healthcare’s wish list since the introduction of electronic health records (EHRs).
The ability to share documentation easily between all of the entities providing patient care (primary care physicians, specialists, hospitals/health systems, physical therapists, long-term care facilities, assisted living communities, home health workers, etc.) has always been viewed as essential to delivering high quality, cost-effective care. Additionally, it’s vital to the transition to value-based care.
Much work has been done, particularly on the part of EHR vendors, to enable interoperability at the enterprise healthcare system levels. Large health systems and hospitals have taken advantage of existing networks like Direct and frameworks like Carequality to start to bring broad-based interoperability to the marketplace. They have made the investments to implement health information exchange, with the goal of improving care coordination and care delivery.
However, a gap remains, specifically for the independent physicians, small practices and post-acute providers –skilled nursing, assisted living, behavior health, therapies and others— who often have limited budgets and staff resources, yet still need access to secure patient document exchange to achieve optimal patient outcomes throughout the care continuum. These providers are critical cogs in the wheel of healthcare and represent a significant portion of bringing a patient through to a positive outcome...yet they’re the toughest to reach.
They’re also the ones for whom a point-to-point HL7 integration project is the least practical or affordable. One reason is that HL7 doesn’t scale easily. If the goal is to have a single snapshot of all care delivered everywhere, it’s crucial that the records of the entire episode of care, including post-acute, become part of the interoperability ecosystem.
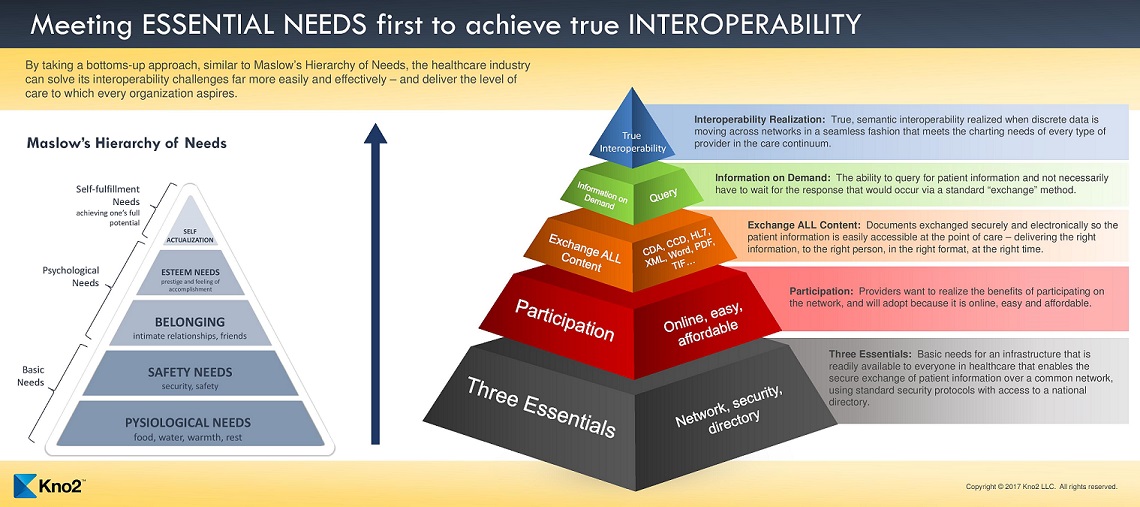
Perhaps the way to do that is to take a cue from psychologist Abraham Maslow’s Hierarchy of Needs. In other words, start with the most fundamental needs -- those shared by every provider. Once those foundational needs have been resolved, we can then address the remaining gaps to achieve full interoperability.
The bottom layer of Maslow’s pyramid focused on basic needs such as food, water and shelter. Until you’ve fulfilled those basic requirements for survival, none of the rest really matters.
The views, opinions and positions expressed within these guest posts are those of the author alone and do not represent those of Becker's Hospital Review/Becker's Healthcare. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them.
