The foregoing observation and proposed corrective action by Lawrence Weed, MD, encapsulate the attitude and approach that differentiate medicine from other professions. But, although generally accepted standards for managing care and clinical information are evolving, suitable information technology (IT) for the automation of standards-based practices in a physician-friendly manner has yet to be offered for use. Electronic health record (EHR) systems are critical “systems of record” but fall short of the customizable clinical cognitive support needed for the mitigation of medical mistakes, which exceed 400,000 instances annually in the United States alone and precipitate more than 210,000 patient deaths.2
Human factors require clinical cognitive support
Human factors analysis (also referred to as human factors engineering) is an essential step in designing equipment, procedures, tasks, and work environments; because research shows that human failures cause 80% to 90% of errors. “The most common root causes of sentinel events are human factors, leadership, and communication,” says Ronald Wyatt, MD, medical director, Office of Quality and Patient Safety at The Joint Commission. “And I argue that leadership and communication are also human factors.”3
Routine work is predictable; knowledge work is unpredictable. Healthcare provider work includes both types, wherein human cognitive capacity often is exceeded because the activities are or include:
1. unpredictable in their execution
2. driven by unknown events
3. actions with unforeseen consequences
4. ad-hoc inclusion of new actors
5. actor knowledge that cannot be encoded in rules and flows
6. unknown inbound and outbound content
7. need for secure, auditable social interactions of actors
8. actor authority/ability assignment based on “need-to-know”
9. complete transparency and auditability 4
Some means is required to minimize human errors by reinforcing the cognitive capabilities and characteristics that healthcare providers need for complete, accurate and timely execution of medical and healthcare processes. However, the currently recommended industry agnostic approach of Lean/Six-Sigma methodologies, a variation of which is The Joint Commission’s Robust Process Improvement® or RPI® process5, tends only to exacerbate the cognitive overload problem. These methodologies require the comprehension and memorization of detailed procedural documentation for subsequent implementation in the healthcare delivery environment, fraught with critical and complex situations. However, IT can deliver the required cognitive support in a manner that leverages available IT system resources and provider-preferred workflows.
IT-enabled clinical cognitive support
What has no suitable IT solution to the clinical cognitive support problem been adopted? The first reason lies with the state of the healthcare IT market: “It is a widely accepted myth that medicine requires complex, highly specialized IT systems… But we need now to take the next step: fitting EHRs into a dynamic, state-of-the-art, rapidly evolving information infrastructure – rather than jamming all healthcare processes and workflows into constrained EHR operating environments …”6 The second reason lies with the IT attitudes and (non)actions of healthcare providers: “The IT foundation required for healthcare is the core set of health data types, the formalization of healthcare workflows, and encoded knowledge (e.g., practice guidelines, decision-support tools, and care plans). With those ingredients, existing … flexible software can support the automation of biomedical processes [emphasis added] … Healthcare is ripe for this approach.”7
We agree that “… flexible software can support the automation of biomedical processes …” and also can provide the much-needed clinical cognitive support. Furthermore, we posit that IT-enabled support is the most if not the only cost-effective means to mitigate the currently unacceptable incidence of medical mistakes and consequent patient adverse events; but only if it is configured and deployed in a manner appropriate for direct use by healthcare providers at any time and place. The following definition and supporting paradigm shift descriptions of adaptive case management (ACM) are directly applicable to the medical practice and healthcare provider domains:
… an information technology that exposes structured and unstructured business information (business data and content) and allows structured (business) and unstructured (social) organizations to execute work (routine and emergent processes) in a secure but transparent manner involving three distinctive paradigm shifts:
1, ACM is a productive system that deploys not only the organization and process structure but through backend interfaces becomes the system of record for the business data entities and content involved;
2, ACM enables non-technical business users in virtual organizations to seamlessly create/consolidate processes from business entities, content, social interactions, and business rules;
3, ACM moves the process knowledge gathering in the life cycle from the template analysis/modeling/simulation phase into the process execution. The ACM system collects actionable knowledge … based on process patterns created by business users.8
Therefore, IT-enabled ACM can meet the needs of healthcare provider knowledge workers by providing the necessary scope and strength of cognitive support; but only if implemented using the most appropriate commercial off the shelf (COTS) architecture and platform. The required architecture is the intelligent business process management suite (iBPMS). “iBPM is the natural evolution of the earlier BPMS [business process management suite] market, adding more emphasis on support for greater system and human intelligence within business processes. Capabilities such as ‘what if’ process simulation, optimization and the ability to gain insight into process performance have been included in many BPMS offerings for several years. iBPMSs have added enhanced support for human collaboration, integration with social media, mobile access to processes, more analytics and real-time decision management.”9 The most appropriate platform is “the cloud,” which term describes an Internet-accessible shared IT system and software facility a.k.a. data center; professionally developed and managed by a cloud service provider (CSP) vendor that can meet contractually the availability, reliability and security requirements inherent in healthcare provider IT applications. Also satisfied are the healthcare provider operational criteria of anywhere and anytime access via a mobile or any other digital devices with Internet connectivity.
In summary, then, clinical cognitive support requires a cloud-based iBPMS including all the software components needed to implement the full scope functionality on a use case-specific basis using collaborative tools requiring minimal IT professional support: a Ci BPMS.
Cognitive support case study
The following case study of a fatal Patient Safety Sentinel Event, described in an article entitled “Human Factors Analysis in Patient Safety Systems” appearing in a recent edition of a publication of The Joint Commission. The case provides a typical opportunity for patient safety optimization using IT-enabled cognitive support as described above:
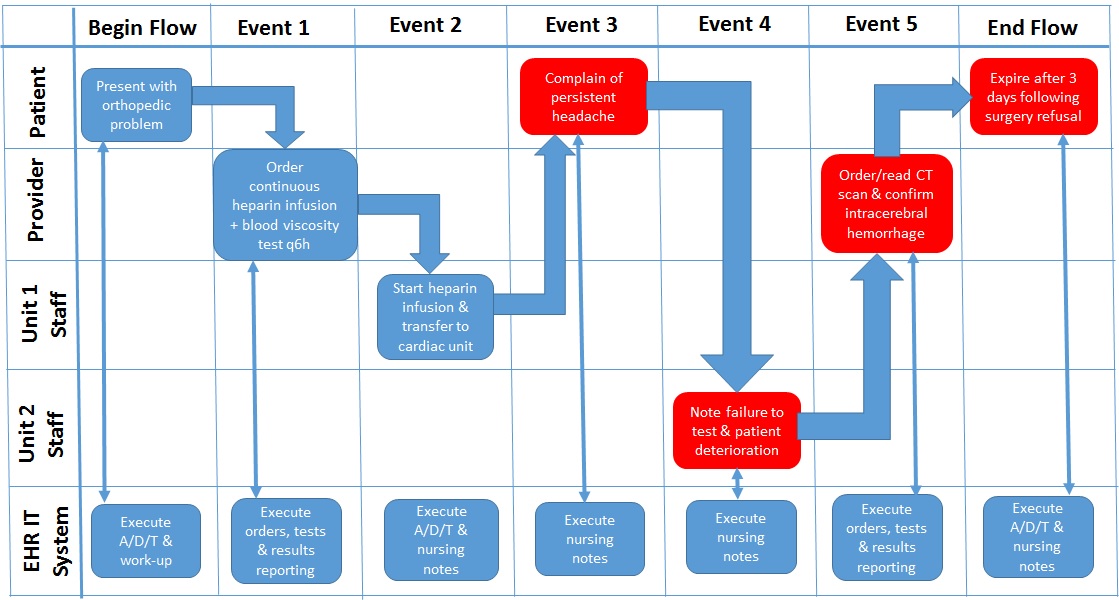
A health care system submitted a root cause analysis (RCA) to The Joint Commission for a sentinel event that involved a patient whose blood levels were not drawn frequently enough to monitor the thinness of her blood while receiving a continuous heparin infusion. The patient had been started on a heparin infusion on an orthopedic unit and then was later transferred to a cardiac unit. The order set for the heparin infusion was not entered properly, leaving out the automatic order for blood tests every 6 hours. During the handoff report, the nurses did not discuss when the next blood test would occur to monitor the heparin infusion. For 24 hours, the patient went without blood tests until an oncoming nurse questioned the situation during the handoff report. At this time, the off-going nurse also reported that the patient had been complaining of a headache for several hours. A computerized tomography (CT) scan showed intracerebral hemorrhage. When the patient’s mental status deteriorated, the family chose not to proceed with surgery due to the patient’s multiple comorbidities and recent decrease in quality of life. She expired three days later. Although the organization had conducted a thorough RCA, The Joint Commission asked it to revise the RCA and consider human factors issues that led to the event and implement more strategies that incorporate human factors solutions, which would more reliably prevent the event from occurring again.10
The patient monitoring fatal sentinel event activity flow described in foregoing case study is depicted the “As Is” process diagram in Figure 1.
Figure 1 – “As Is” Manual/EHR-Supported Patient Monitoring Process
If however, a CiBPMS had been available either on-site at the reporting healthcare system premises or by subscription to the solution as a service, then such a tool could have been specified in The Joint Commission’s Patient Safety System Standard. Therefore, the Commission could have required an automation of the patient monitoring use case as a specific strategy in its request “… to revise the RCA [root cause analysis] and consider human factors issues that led to the event and implement more strategies that incorporate human factors solutions, which would more reliably prevent the event from occurring again.” Subsequently then, the CiBPMS-developed automated use case would be running continuously and/or conditionally per its healthcare provider SME-specified design. For the next instance of patient monitoring as described in the RCA report, CiBPMS-created automated use case could have recognized the failure to perform blood viscosity tests q6h, alerted staff of the omission, and prevented the patient’s death. This “To Be” process is depicted in Figure 2.
Figure 2 – “To-Be” CiBPMS-created Patient Monitoring Process
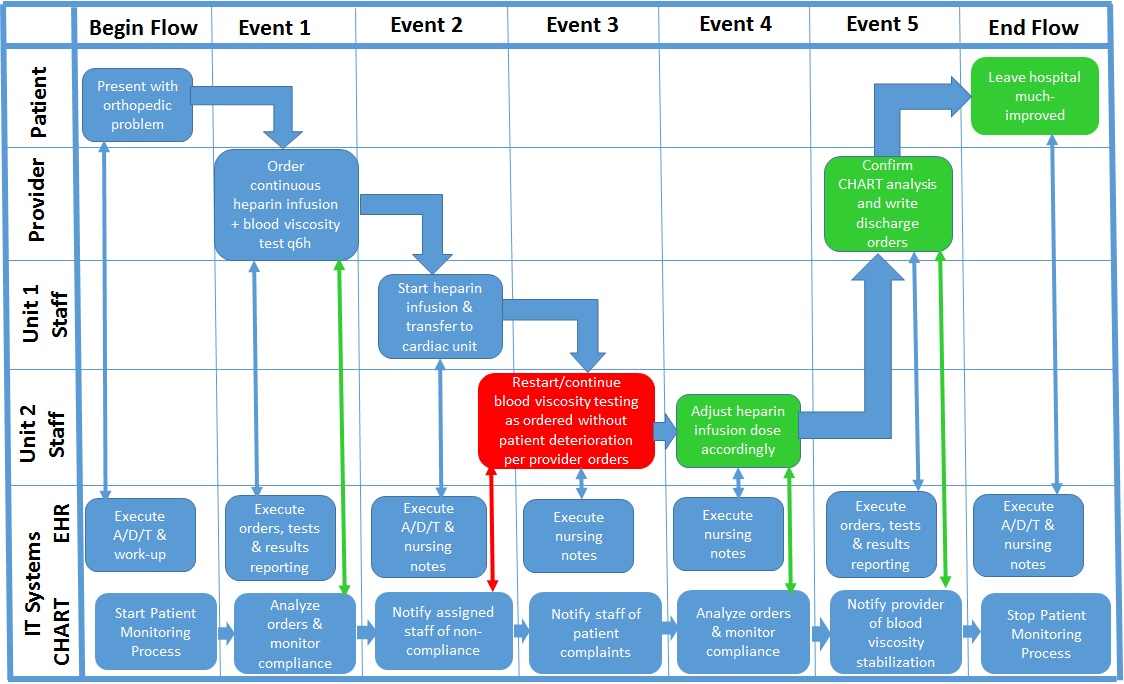
Reliable medical mistake mitigation and consequent patient adverse event avoidance require clinical cognitive support that only a CiBPMS can create, if employed by innovative healthcare provider subject matter experts.
N.B. – The authors and other Directors and Professional Advisory Board members of CHARTSaaS.org, a U.S. IRS 501(c)(3) corporation, seek tax-deductible funding for development of the Cloud Healthcare Appliance Real-Time (CHART) Solution as a Service, a CiBPMS for subscription service for licensed/accredited healthcare providers (re www.chartsaas.org).
1 Weed, LL, Weed, L. Medicine in Denial, April 2011 (www.createspace.com/3508751). Dr. Weed invented the problem-oriented medical record, the SOAP clinical documentation method, and patient problem-knowledge coupler technology.
2 http://journals.lww.com/journalpatientsafety/fulltext/2013/09000/a_new,_evidence_based_estimate_of_patient_harms.2.aspx
3 The Joint Commission, The Source, Human Factors Analysis in Patient Safety Systems, XIII:4, April, 2015, p. 1, http://www.jointcommission.org/assets/1/6/HumanFactorsThe_Source.pdf
4 https://acmisis.wordpress.com/what-is-adaptive-case-management-acm/
5 The Joint Commission Center for Transforming Healthcare, http://www.centerfortransforminghealthcare.org/about/rpi.aspx
6 Mandl. KD, Kohane IS. “Escaping the EHR Trap – The Future of Health IT,” N Engl J Med 2012; 366:2240-2242, http://www.nejm.org/doi/full/10.1056/NEJMp1203102?viewType=Print&viewClass=Print
7 Ibid.
8 Workflow Management Coalition, http://www.xpdl.org/nugen/p/adaptive-case-management/public.htm
9 Gartner, https://www.gartner.com/doc/reprints?id=1-2BYYFBE&ct=150319&st=sb&elqaid=896&elqat=2&elqTrackId=664384b2119a4628b31126e195625b64
10 The Joint Commission, op.cit.
The views, opinions and positions expressed within these guest posts are those of the author alone and do not represent those of Becker’s Hospital Review/Becker’s Healthcare. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them.
