In addition, hospitals & doctors are sending patients to nursing homes unnecessarily, and have been for years. In fact, it became the norm many years ago.
My mom, bless her heart, has stage seven Alzheimer’s Disease. In my case, being a former hospital CEO and now a caretaker, the inadequacy of this process has become very clear.
First, doctors often advise patients and their families that the patient is being “transferred” to a rehab facility to recover. The word transfer suggests the care plan is mid-stream and not complete. For example, if the doctor stated “your mom is being discharged from the hospital to a nursing home,’ the word discharge suggests more finality and perhaps a choice in discharge location.
Second, there is much confusion about the different levels of post-acute care. Patients and families are often told they are going to a rehab facility, only to discover later that the term “rehab facility” is synonymous with “nursing home” in many cases.
Third, hospitals have failed miserably in clearly communicating to families that they not only have a choice in which post-acute facility to choose, but the choice to go to a post-acute facility at all. It is the hospitals responsibility to communicate this to the family and educate them on the risks of going home to recover.
Fourth, patients are often referred to more expensive, higher levels of care after the hospital that may be inappropriate, simply because their insurance benefit pays for the service. This is especially true with Medicare patients who for years have been referred inappropriately to log term acute care hospitals, acute rehab hospitals and nursing homes, simply because they are a “covered benefit.” For hospitals, doctors and case managers this simplified the discharge process and helped shorten length of stay. In short, it was the path of least resistance to get patients out of the hospital quickly, which led to increased profits for doctors and hospitals.
I can admit that as a hospital CEO I was guilty of pressuring case managers to get patients discharged as quickly as possible. I am also willing to acknowledge that this pressure led to bad habits and patterns which became the norm. Will other executives and case managers around the country who are reading this story look in the mirror and take the same accountability?
So to summarize these four points: Patients are often being sent to post-acute institutions unnecessarily, and are not being educated thoroughly enough about post-acute options because the incentives for hospitals, doctors and case managers to communicate and educate thoroughly contrast the hospitals financial incentives.
Until now. The rules have changed. Those hospitals and health systems who don’t acknowledge these bad habit and create a plan to address them will suffer the financial consequences.
As CMS forces health systems in to Accountable Care Organizations and Bundled Payment programs, the health system is now at-risk and the make-shift payer. In many cases nowadays, every dollar spent on post-acute care is a dollar spent by the health system.
The rapid increase in value based reimbursement has led to soft-steering by hospitals and doctors to preferred post-acute providers. It has also led to hospitals taking a “home-first” mentality when discharge planning. A stark contrast to the “path of least resistance, send them to a nursing home” approach of the fee for service era.
Thus, after ten years as a hospital CEO and health system Vice President overseeing home health and hospice services, with previous experience as a nursing home administrator, I designed the Discharge with Dignity Model and introduced it to 3,000 case managers from across the country during my keynote presentation at the Case Management Society of America Annual meeting.
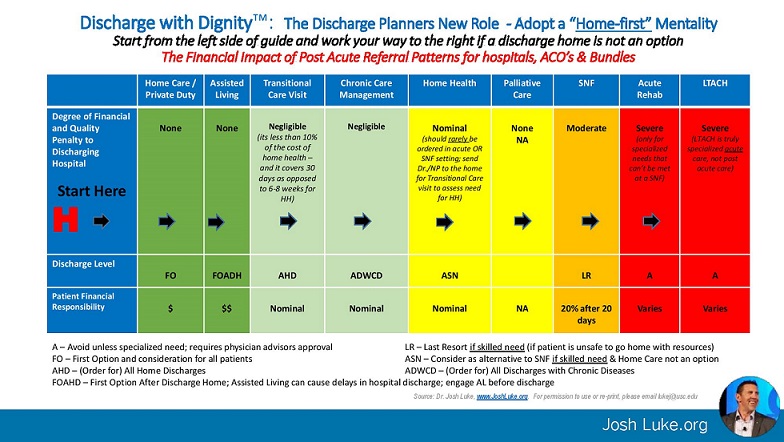
I introduced the Discharge with Dignity model and guide as a means to end these practices and invoke cultural change in health systems. Discharge with Dignity is a guide designed to accomplish two specific goals: 1) Remind case managers that every American prefers to age and heal at home; 2) Remind case managers of the financial penalties assessed on hospitals and health systems for over-utilizing post-acute institutions.
You can see the guide by clicking on: https://www.linkedin.com/pulse/doctors-hospitals-sending-seniors-nursing-homes-your-mom-luke-ph-d-
The guide was developed as a tool for case managers in the hospital to start on the left (discharge home) and rule out each option before even considering the next option to the right. As you move to the right, post-acute options become more expensive, ultimately ending with the ultra-expensive post-acute options of long term acute care and acute rehab in red on the far right.
If the hospital discharging patients sends a high volume of patients to one of these red level facilities, long term acute care or acute rehab, the hospital will likely be fined or have reimbursement reduced as a result of their accountable care organization, bundled payment program or Medicare Spending Per Beneficiary penalty. A triple whammy.
One fact remains constant even as we transform to a home-first mentality: Every patient should be looked at individually based on their needs and their home environment. We often refer to this as “right care, right place, right time.” Since adopting Discharge with Dignity and this home first mentality, hospitals have begun partnering with non-medical home care franchises, or in some cases (St. Josephs Health System in Orange, Calif.) buying its own home care franchises. Why buy though? AMADA Senior Care in San Clemente, California has seen rapid national growth since it announced its DART Readmission Partnership program that is offered at no cost to the hospital. Its willingness to allocate an entire full-service franchise team to a single hospital to expedite discharge by offering a full scope of low-cost senior services for those who choose to recover at home has been well accepted by hospitals who have proven unwilling to pay for these services.
The diagram does come with the reward of improved patient satisfaction, and a more financially viable health system when implemented correctly. Discharge with Dignity was designed because my mom is the patient. She deserves to be educated and communicated to about her options. So does your mom.
Dr. Josh Luke is a veteran hospital CEO and health system Vice President, award winning post-acute strategist and serves as Adjunct Faculty at the University of Southern California, Sol Price School of Public Policy. He is a social media influencer on LinkedIn and Twitter and founded the National Readmission Prevention Collaborative. He is the closing keynote presenter at Becker’s Hospital Review 6th Annual CEO + CFO Roundtable in Chicago in November. 2017. Luke is also the author of two book, Readmission Prevention and Ex-Acute.
The views, opinions and positions expressed within these guest posts are those of the author alone and do not represent those of Becker’s Hospital Review/Becker’s Healthcare. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them.
