While NY’s Empire is one of the largest non-profit Blues in the US, Anthem Wellpoint (for profit) is one of the largest Blue plans in the US with over a dozen states in their BCBS span of control.
Pre-payment audits are more onerous than post payment because the payment for the services is suspended while the medical record is reviewed by (let’s hope) certified coders. This review process may take weeks or months while the practices accounts receivable continue to age for these services.
Both Empire and Anthem announced their audits in December 2015 Bulletins, Anthem’s pre-payment review appears at this time to be limited to their Medicare Advantage products. According to several knowledgeable sources, Anthem will compare the Level V codes against their newly revised (but as yet undisclosed) ICD-10 diagnosis list of “approved Level V” services. If the ICD-10 code choices by the ED group do not match the Anthem list, Anthem will request the ED records and begin the pre-payment and medical record review of the provider’s code choices. See Myles Riner, MD and his blog here.
While the expected length of a group’s or physician’s audit period is not specified in the their respective bulletins, ED groups and clinicians are wise to keep close track on the length of time a particular physician or group is under review. As in the past with Medicare post payment reviews, after a reasonable period of time and successful defense of the code choices, the message of “enough is enough” to the BCBS medical director should be communicated by the ED group practice representatives.
Recently announced by Palmetto Railroad Medicare, Railroad Medicare’s Medical Review (MR) unit will begin a service-specific review of Evaluation and Management (E/M) CPT code 99285, emergency department visit, requiring high complexity medical decision making.
Palmetto states that E/M 99285 was selected based on internal data analysis. At the conclusion of their review, Palmetto has stated it will publish the findings on its website. Below is detailed information from Palmetto about how it will approach the audit preparation.
Preparing for the Review
Palmetto reminds providers, regardless of claims selected for review, of various coverage guidelines which would require the following:
- The medical necessity and appropriateness of the diagnostic and/or therapeutic services provided:
- Medicare allows only the medically necessary portion of the ED visit. Even if a complete note is generated, only the necessary services for the condition of the patient at the time of the visit can be considered in determining the level/medical necessity of any service.
- Palmetto is cautioning here against “buffing the chart” simply to potentially obtain higher level E/M scoring.
- That services furnished have been accurately reported
- Recall that the CMS 1500 claim has “certification” requirements by the provider that all information is “true, accurate and complete.”
- The medical record should be complete and legible, and documentation for each patient encounter should include the following as clinically relevant and appropriate given the patient’s presentation to the ED:
- Beneficiary name
- Date of service
- Reason for the encounter (Chief Complaint) and relevant history, physical examination findings, and prior diagnostic test results
- Assessment, clinical impression, or diagnosis
- Past and present diagnoses
- Beneficiary’s progress, response to and changes in treatment, and revision of diagnosis
- Diagnosis and treatment codes reported
- Appropriate health risk factors
- Medical plan of care
- Rationale for ordering diagnostic or other ancillary services
- Legible name and signature of the rendering provider, including credentials
There May Be Relief to the Medicare Appeals Delays: “On the Record” Reviews
The PBS Newshour reported that in May 2015, the average provider appeal took over 572 days to complete; today, the situation is not greatly improved but it is believed that these average processing delays have decreased.
There are generally 5 stages to a Medicare appeal as shown here:
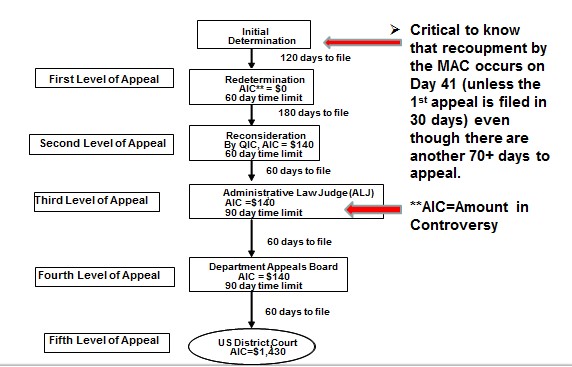
First, to avoid automatic recoupment by the Medicare MAC, the provider’s appeal should be filed within the first 30 days; if the provider waits the additional 60-70 days to file its appeal, the Medicare MAC will recoup the alleged overpayment and the provider is left with a many year appeal process in front of them to reclaim their reimbursement. So be prompt and thorough with the appeal response.
Second, to relieve the appeals backlog, the DHHS Office of Medicare Hearings and Appeals (OMHA) began a pilot project of “on the record reviews” (OTR) in July 2015. OTR legal reviews have been around for decades in other legal settings and are even used at the US Supreme Court. The appellant simply states that oral argument is not requested and that the reasons for the appeal are completely stated “on the record”, meaning the written appeals record. Not having oral argument and the briefing that is required for oral argument saves the adjudicator and litigants valuable time. In sharp contrast to the over 570 day average appeal time reported in May 2015, the average OTR appeal is approximately 57 days.
Conclusion
OMHA is experimenting with mediation and other tools to address the huge appeals backlog created in response to aggressive Medicare RAC and MAC audits of providers. While the RAC program may be entering new phases of growth and development, ED groups should remain vigilant as BCBS plans (Empire and Anthem) and the Medicare MACs like Palmetto Railroad Medicare begin to draw a laser focus on CPT 99285 services—and being fore-warned is being fore-armed.
The difference this time is that Anthem’s audit program has clearly introduced the “X factor” of using a newly revamped “ICD-10” diagnosis list (as yet to be seen or determined by the provider community) for so-called “approved CPT 99285s”. Here, what’s old is new again—we recall with no particular fondness the “approved ED diagnosis lists” of the early 1990s which were used to block or thwart appropriate ED reimbursement particularly with Medicaid managed care. EDPMA and ACEP’s strong lobbying for the “Prudent Lay Person” Amendments to the Balanced Budget Act of 1997 on balance effectively dealt a blow to such diagnosis lists but that was ICD-9 then and now we have 5 to 6 X of the number of codes with ICD-10—so here we go again.
References
Railroad Medicare Hub, “Medical Review Pre-payment Review of Evaluation and Management Code of Emergency Department Visit, with Highly Complex Medical Decision Making” http://www.palmettogba.com/palmetto/providers.nsf/ls/Railroad%20Medicare~A6JLW22623?opendocument&utm_source=RRBL&utm_campaign=RRBLs&utm_medium=email
