Healthcare providers under regulatory and financial pressures are pursuing significant and urgent organizational changes, making collaboration among clinical and administrative leaders more important than ever.
"There are tremendous inefficiencies in care and cost, including clinical variations, that without physicians as a true partner you will not be able to resolve," said Dr. Morris Seligman, executive vice president/chief medical officer of Mountain States Health Alliance, based in Johnson City, Tennessee. "Those who lag in aligning physician and administrative goals will risk poor clinical and financial outcomes."
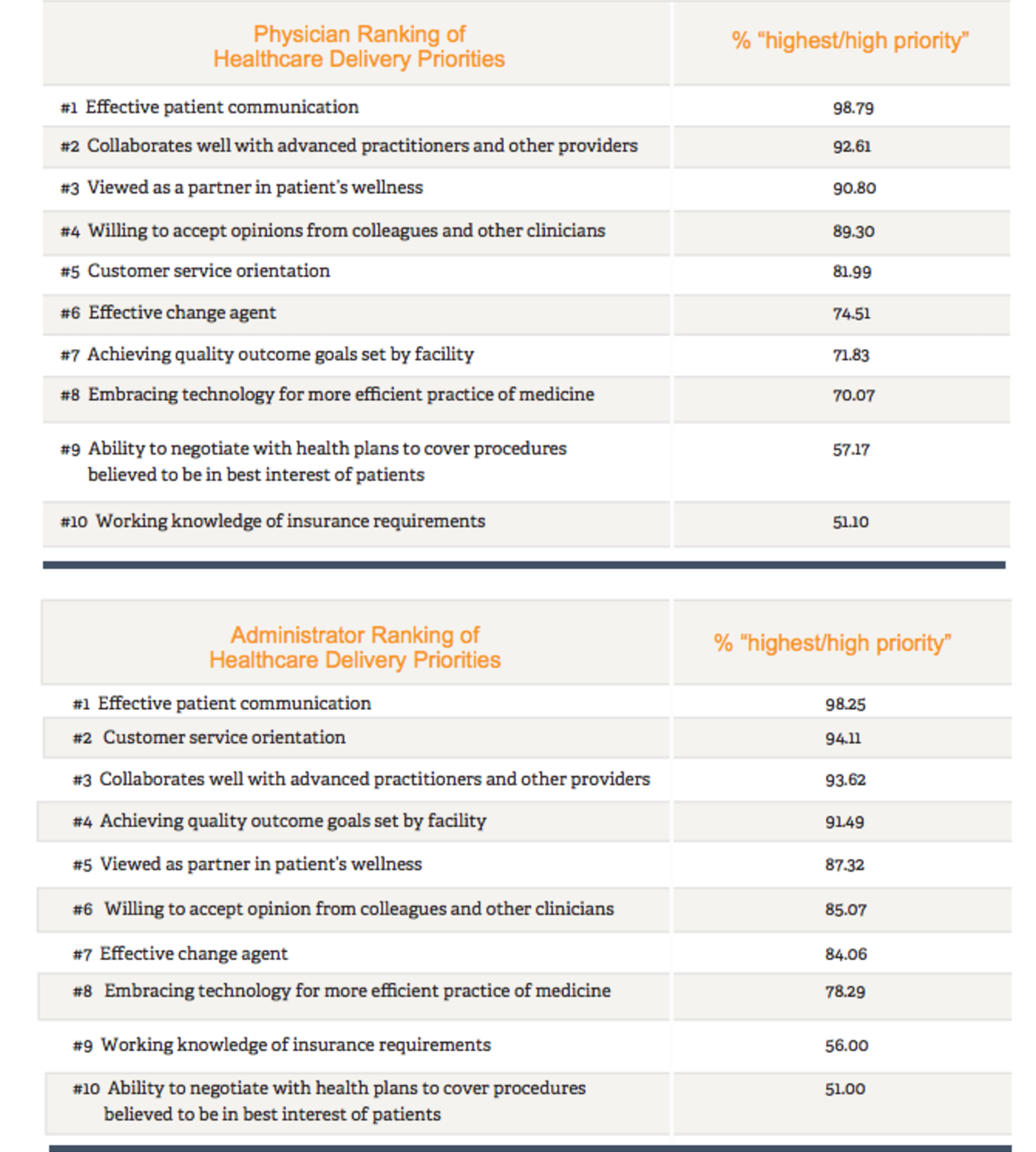
A 2016 study by Cejka Search of 1,621 U.S. practicing physicians and healthcare administrators explored how physicians and administrators view a set of ten healthcare delivery priorities. The study found the two groups to be closely aligned on the highest priorities, as well as the lowest which centered on working with insurance carriers and embracing technology.
Patient communication and collaboration emerge as highest priorities
The highest priorities were "patient communication" and "collaboration with other providers," indicating strong support for a team-based approach to care with the patient as the focus. Even where the top three rankings differed there was a common theme of the patient experience, according to Cejka Search President John Gramer. "Physicians were focused on collaborating with patients to achieve long-term wellness, while administrators took the broader view of overall patient satisfaction."
Perceived gap in how well doctors communicate
A gap arose when asked how effectively physicians communicate with patients:
• Ninety-four percent of physicians rated themselves as very good or good
• Sixty-two percent of administrators rated the physicians at their facility very good or good
Dr. Thomas Diller, vice president and system chief medical officer of CHRISTUS Health in Irving, Texas, believes that many patients wanting to please their doctors fail to speak up when something is misunderstood. Therefore, doctors have to be trained to ask for these signals. Simulated patient communication and empathy training conducted last year for all employees of Virginia-based Sentara Medical Group employees is one of the tactics its president, Dr. Doug Culling, credits with increases in patient satisfaction scores.
Need for more meaningful definition of quality
Additionally, quality programs emerged as a significant opportunity for improved alignment between the two groups. Although physicians in the study showed strong support for a value-, versus volume-approach, they want more meaningful definition and measurements of quality. One physician explained, "We risk quality when we focus on desired outcomes that are not founded on medical evidence." As a result, there was a twenty-point difference in how important administrators and physicians viewed "achieving quality metrics set by your facility:"
• Ninety-two percent of administrators said high/highest priority
• Seventy-two percent of physicians said high/highest priority
The Centers for Medicare & Medicaid Services and other external entities' metrics have encouraged a "check-the-box" approach to quality that adds little value in the context of the physician-patient relationship, explained Diller. As a result, physicians are frustrated with "meaningless" over-measurement and administrators are on the hook for value-based purchasing that demands it.
Outcome, not process of care matters most
Physician executives said the answer is for providers to take the lead in extending their quality programs beyond the CMS guidelines to also include metrics that capture the outcome of care and not just the process. "In addition to the number of foot or eye exams diabetics receive, we need to be measuring the number of patients who have their diabetes under control and are able to avoid life-limiting and costly complications, such as amputation, dialysis and blindness," said Seligman.
Engage physicians in the process
Whether the goal is improving quality outcomes, reducing cost or improving the patient experience, physicians want to be treated as a partner in the process. "No one is more qualified than physicians to determine how to deliver care efficiently," said one practicing physician. Another added, "We are open to change; we just need to understand why something is required before we buy-in."
Industry experts agree that physician involvement in setting goals and designing solutions in partnership with operational leaders is the best way to achieve meaningful clinical and operational change. Those who have the right clinical and administrative leaders in place to build a culture of collaboration that is founded on alignment of goals and priorities will succeed.
About the author
Leveraging twenty-five years of healthcare experience, Paul Esselman consults with healthcare organization boards and committees on senior-executive search engagements and assists with organization development and succession planning strategies.

