Driscoll Children’s Hospital in Corpus Christi, Texas is a tertiary care, regional referral center offering complex and comprehensive medical and surgical care for children. Our location near the Gulf of Mexico makes high humidity a frequent issue. Was someone’s nose just working overtime or was there really a problem? What if the smell was indicative of a greater issue with mold, bacteria or fungus, any of which can trigger hospital-associated infections (HAI)?
 The CDC considers hospital-associated infections to be a threat to public safety, reporting nearly three-quarters of a million HAIs in hospital patients. More than 75,000 people with HAIs died during their hospitalizations. The problem is real, growing, and urgent. We didn’t have an outbreak of infectious disease, but weren’t willing to wait until an outbreak occurred.
The CDC considers hospital-associated infections to be a threat to public safety, reporting nearly three-quarters of a million HAIs in hospital patients. More than 75,000 people with HAIs died during their hospitalizations. The problem is real, growing, and urgent. We didn’t have an outbreak of infectious disease, but weren’t willing to wait until an outbreak occurred.
We launched a comprehensive internal investigation of sourcing and air sampling, then designed and conducted an evidence-based pilot to confirm and resolve air quality issues. The study reflected the impact of an active environmental air treatment system with an ultraviolet germicidal irradiation chamber on neutralizing airborne pathogens. The pilot resulted in a 73 percent decrease in the total airborne bacteria count and a 44 percent decrease in airborne fungal counts.
First steps
Before we initiated the study, we tried to source and solve the musty odor problem. Over the course of 10 weeks, our teams looked top to bottom, from fan coils in patient rooms to sink drains, but no leaks were found. Our engineers reinforced the walls over drainage lines to see if that would correct the problem. It did not.
They looked at the air conditioning lines in the ceiling, and found condensation due to the temperature differences between the warmer air and the cold lines. They installed fans in the ceiling, but that solution caused its own set of problems, so the fans were removed. And the smell lingered.
Because we couldn’t locate a physical source for the odor, we turned to the air. Air sampling revealed new issues: we learned what pathogens were in the air, and how many. But were the number and type of organisms unacceptable? That was undetermined, because we discovered there are no universally accepted standards for air quality in medical facilities. The industrial hygienists we consulted had differing opinions, so we created our own standards for the air quality in patient rooms.
We’re a children’s hospital and see patients from birth to age 21. Some are especially sick: some are immunocompromised, some have had transplants, some have cancer, and some have had cardiac surgery. This patient population is already at increased risk, and they’re under our care. We wanted to offer them greater protection.
Cleaning the air
Cleaning a patient room in a hospital starts with surfaces. All people shed bacteria constantly, and these bacteria collect on bed rails, light switches, sinks, even bed linens. Fungus settles out of the air and lands on surfaces as well. These surfaces are all cleaned according to a strict protocol. We even employ an ultraviolet light to spot check surfaces for cleanliness. But what about the air? How do you clean something you can’t even see?
Again, the answer is ultraviolet light. Although hospitals have understood the benefits of ultraviolet germicidal irradiation (UVGI) and used it for decades, there have been challenges to implementing this technology. A surface had to be in the direct line of the light in order to be cleaned. It couldn’t be used in an occupied space, and as soon as cleaning was complete, pathogens could begin to accrue again through settling. And the devices were expensive. We wanted to use this technology to clean the air itself.
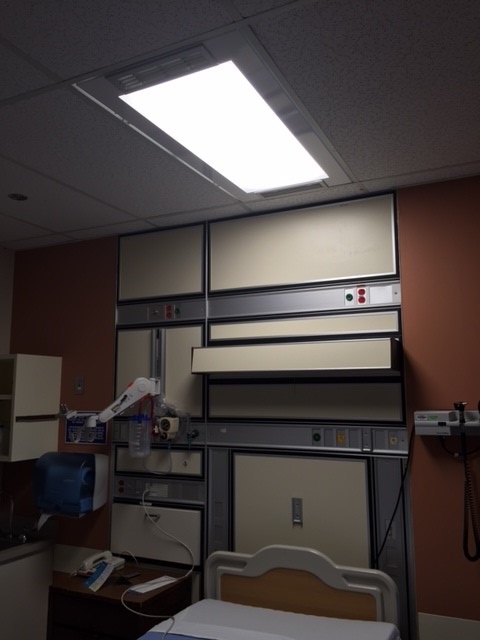
Enter the Health Risk Management System, where the HRMS UV-C/UVGI mechanism is housed atop a standard footprint (2 x 4) ceiling light fixture. Because the ultraviolet light itself is completely shielded, the room does not need to be vacant, and, in fact, can operate 24/7 in an occupied room. Each unit houses four small fans (like those in a laptop computer) that pull room air into the system at 50 cubic feet per minute. The air passes through the irradiation chamber, and then the cleaned air is pushed back into the room. The intake and exhaust vents are set at a 30 degree angle, which moves the air in a pattern that avoids repeatedly recirculating the same air.
The pilot
When we determined that cleaning the air was a reasonable next step, we set about designing a pilot study with Dr. Linda Lee, DrPH, MBA of American Green Technology. A room at Driscoll would be selected, and the air sampled for an independent testing agency to culture and report its findings. Then the HRMS lighting/air treatment units would be installed, and later further sampling and testing conducted and the results compared. It was a way to objectively measure which and how many contaminants were in the air, and whether and how well the active UV-C air treatment units worked to reduce the levels of contaminants in the air.
 For the study, we selected patient room 425 on the fourth floor oncology unit. The room of approximately 220 square feet was vacant and had been terminally cleaned and was under positive pressure. Pre-installation sampling was done by running the SAS 180 sampler to pull 1000L of air through it onto agar plates specific to collect bacteria and separate agar for fungus.
For the study, we selected patient room 425 on the fourth floor oncology unit. The room of approximately 220 square feet was vacant and had been terminally cleaned and was under positive pressure. Pre-installation sampling was done by running the SAS 180 sampler to pull 1000L of air through it onto agar plates specific to collect bacteria and separate agar for fungus.
When 30 samples for bacteria and fungus had been collected over two days, the plates and chain of custody documents were packaged under refrigerated conditions and shipped overnight to the independent lab for incubation. All plates were incubated for 5-7 days, after which they were evaluated. An error correction, standard in the industry, was performed for all air sampling samples, using the SAS 219-Hole Impactor Correction Factor.
After two active UV-C air treatment units were installed in patient room 425, post-installation sampling following a similar protocol for bacteria and fungus was conducted. The only difference in the room conditions was that a patient had been in the room (on isolation) and the room had not been terminally cleaned.
The findings
“The air in the patient room is quietly pulled into the UV-C chamber and continually treated, 24 hours per day,” said Dr. Lee. “It was very satisfying to improve the conditions in the room, and to improve the environment for everyone; patients, staff, and visitors.” The results reported from the lab were impressive. In patient room 425, total bacterial count in the air was reduced an average of 73 percent and fungal counts were reduced by 44 percent. “These values are especially notable because the room had been occupied until two hours before the post-test sampling began by an isolation patient,” Dr. Lee said. “The room had not yet been terminally cleaned when post-installation commenced, so it is reasonable to assume that bacterial counts would be quite high at the time of post-installation sampling.”
Just to be sure, we ran another post-installation test, to see if our results matched the reporting. The results were good. The data from the research pilot supports our incorporating an active UV-C air treatment system in our HAI prevention protocol as a great adjunct to our infection control efforts. The continual cleaning of the air is a terrific investment for our patients and their welfare.
And that musty odor? Along with the bacteria and fungi, it’s gone, too.
About the author
Nancy Fallwell, RN, MSN, MHA is director of Infection Prevention & Control at Driscoll Children’s Hospital in Corpus Christi, Texas. Fallwell was formerly the interim director of Infection Prevention & Control and, prior to that, was a nursing house supervisor at Driscoll. She has served in various nursing roles at Corpus Christi-area hospitals, the first as a nurse technician at Driscoll in 1989. Fallwell holds a master’s degree in nursing and healthcare administration from the University of Phoenix and a bachelor’s degree in nursing from the University of Texas at Tyler.
Add’l Photo:
Installed HRMS unit.
The views, opinions and positions expressed within these guest posts are those of the author alone and do not represent those of Becker’s Hospital Review/Becker’s Healthcare. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them.
