In the comedy classic “Groundhog Day,” Bill Murray plays a Pittsburgh TV weatherman who, during an assignment covering the annual Groundhog Day event in Punxsutawney, Pennsylvania, finds himself caught in a time loop, repeating the same day over and over. In many ways, infusion center staff can surely relate to Murray’s predicament. Patients arrive — some early, some on time, some late — but all wait. And wait. The 10 a.m. to 2 p.m. peak is especially problematic. And this happens every day.
It’s not for lack of trying. For years, infusion centers have experimented with different ways to schedule patients, such as assigning patients to a specific nurse or chair when the appointment is made or to a “pod” of chairs within the infusion center. Others have combined those approaches with an acuity model, spreading appointments among nurses, chairs or pods based on the complexity of the patient’s treatment and condition. And to be fair, some of those approaches have worked — at least temporarily. In most cases, though, it only takes one no-show, one add-on, one patient who reacts negatively to treatment, one nurse who calls in sick, to throw the entire day back into disarray. Of course, an increase in patient volume also renders any previous scheduling scheme null and void.
Why, exactly, doesn’t scheduling to a pod, chair or nurse work? In a problem with multiple key resource constraints, focusing on just one gives a suboptimal answer at best and has the potential to introduce major bottlenecks at worst. Scheduling to a nurse hides the chair utilization, so it’s possible to build a schedule that lines up patient starts well for the nursing team but creates a major peak in chair utilization. Similarly, scheduling to a chair makes it difficult to plan a schedule that will work well for nurses.
On top of that, filling in schedules for a particular resource as each patient need arises means that the schedule is built through a series of isolated negotiations between a patient and a scheduler — without considering the rest of the patient demand that still needs to be booked. To end up with an answer that works efficiently across multiple constrained resources, you need to run a constraint-based optimization that comes up with a set of appointment options that account for the full expected demand, while ensuring that utilization of both chairs and nurses is optimal, and also spacing out patient starts so that the flow through check-in and pharmacy is smooth as well.
And what about pods? Splitting the problem into pods makes it easier to conceptualize the demand on multiple resources, but creating smaller groupings of nurse and chair resources limits efficiency overall and locks you into patterns that may not work once the events of the day hit — late-arriving patients, patients who need to stay in a chair longer than planned and others who need to be urgently added to the schedule. Similar to the way a hotel gives you your room number only during the check-in process rather than at the time of booking, it is best to defer the final binding of a patient to a nurse and to a chair until the time of treatment. This allows you to place patients with the resources that are truly most available at their appointment time, rather than relying on a plan that was made before the natural variation of the day hit.
At UCHealth, we tried every “solution” we could imagine — Excel spreadsheets, process improvement initiatives, you name it, we tried it — before coming to grips with the realization that infusion scheduling was a problem so complex that we simply lacked the resources and expertise to make meaningful, long-lasting change. We turned to a Silicon Valley-based innovator of cloud-based predictive analytics solutions, LeanTaaS, to deploy their iQueue for Infusion Centers solution at one of our centers with 28 chairs and six private rooms. iQueue uses data science and machine learning to create optimized scheduling templates in order to continuously maximize patient flow and chair usage. The results were dramatic:
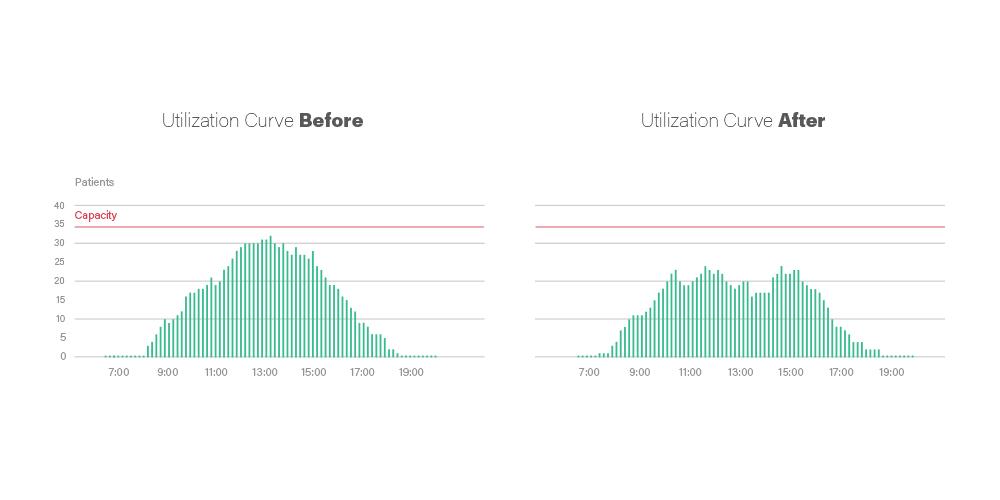
• 33 percent lower wait times at peak hours
• 15 percent lower average wait time
• 16 percent higher patient volumes
• 28 percent lower overtime hours
After realizing these significant results, we deployed the solution at six additional centers and now collectively have 154 chairs leveraging the iQueue platform. Later this spring, we’ll introduce iQueue for Infusion Centers to our three remaining infusion centers.
Does that mean a center is doomed to a Groundhog Day-like existence if they decide scheduling to a pod, nurse or chair is a must-have? Not at all. The iQueue solution can provide pod-specific templates and also has the ability to generate a day-of patient-to-nurse allocation that automatically maps the scheduled appointments to the set of nurses available that day. It’s not a best-of-both-worlds approach though; your center’s overall efficiency will not be as improved as if you had implemented a centerwide optimized template. To escape “Groundhog Day,” infusion centers need to view the appointment duration as the resource to be scheduled against — not chairs, nurses or pods.
###
Jamie Bachman is the executive director for oncology services at the University of Colorado Hospital (a part of UCHealth), the primary clinical site for the University of Colorado’s NCI-Designated Comprehensive Cancer Center. He has over 15 years of leadership experience in academic and community oncology settings. Jamie holds a bachelor’s degree from Ithaca College and a master’s degree from New York University.
The views, opinions and positions expressed within these guest posts are those of the author alone and do not represent those of Becker’s Hospital Review/Becker’s Healthcare. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them.
