Though many ACOs did cut costs, of the 353 ACOs, there were $411 million in total savings, but for most ACOs, it was not enough.
The goal of Medicare’s performance-based reimbursement is to save money and improve outcomes, as illustrated by both the Merit-Based Incentive Payment System (MIPS) and Alternate Payment Models (APMs). However, if ACOs are to be sustainable, they have to deliver on shared savings. It’s not enough to save money; if you have also invested heavily in infrastructure, recouping those up-front costs may wipe out any savings for several years.
How can ACOs break through the barrier to shared savings in the near future? Here are four lessons from analyzing the CMS data:
Lesson 1: Focus on Performance Goals
ACO performance measurement is distinguished from other CMS programs by universal measures and the use of a patient population sample in reporting. There is very little flexibility regarding which patients are included in the reporting sample, and the choice of measures to report is limited. This is in stark contrast to Physician Quality Reporting System (PQRS), where groups doing registry reporting are able to select a set of measures from a larger pool and report on the majority of eligible patients. In short, groups cannot manipulate ACO performance results by choosing the best measure results to report.
Reporting quality is not the issue for ACOs. It may be cumbersome to extract data from the Electronic Medical Records (EMRs) into the CMS tool, but only five percent of ACOs were unable to fulfill reporting requirements in 2014. While this is admirable, it does not solve the shared savings dilemma. Since you are always compared to your past performance for patients on Medicare, you need better results across the spectrum to stand out from the crowd. You will also need to grow your ACO with patients new to Medicare by adding more primary care providers, enriching your pool with new patients to offset the continued downward pressure on costs for the older population of patients you’ve had.
Lesson 2: Leverage Previous Quality Initiatives to Become an Experienced First-Time ACO
The more experienced the ACO, the more likely that ACO will be able to achieve shared savings. The data shows those who started in 2012 were twice as likely to succeed as those who started in 2014. This trend is also apparent when looking at overall savings. Even as those who held spending below their targets saved an additional $100 million between 2013 and 2014, proportionately, the influx of new ACOs has brought the per-ACO savings rate down by nearly a third among those who came in below their estimated costs.
Quality is also improving with time. Over the last year, performance averages improved for 27 of the 33 ACO measures. This is certainly reassuring for the program’s stakeholders, but should also be a wakeup call for those considering creating an ACO. The bar is being raised each year, and the longer you wait, the more difficult it will be to keep up.
You will need to build on your previous experience to catch up to the experienced ACOs. If you have participated in PQRS Performance prior to the ACO, continue your performance measurement of all Medicare patients. If you have used a Registry for reporting quality, you can transition to evaluating patients under ACO measures very easily and capture the underlying data you need, both to report quality and to identify patients for performance improvement efforts.
If you have also performed patient outreach in the past and achieved desired results, such as return visits, screenings, or better care coordination, these can move into your ACO tool set. However, you need to evaluate carefully what produces results, since resources will be limited. A Registry partner with the research capabilities embedded in performance improvement will help you measure the effectiveness of your interventions.
Lesson 3: Use Caution when Considering “Advance Payment”
Succeeding with an ACO takes infrastructure for performance measurement and improvement, an internal governing structure, providers, and staff. This takes time to build and requires a start-up investment. For this reason, Medicare offers an option for “Advance Payment.” By using the Advance Payment ACO Model, groups are able to take out a loan from Medicare, using expected savings as collateral.
Unfortunately, many groups found start-up money doesn’t automatically translate into positive results. The most recent Public Use File shows, of the 36 ACOs which received advanced payment, more than half of them were unable to generate enough savings to cover the amount of Advanced Payment they received, and some actually incurred losses—a double hit.
Lesson 4: Carefully Build Your ACO Network and Initiatives
Why does one ACO succeed and another fail? Does the number of patients, the number of providers or the provider-to-patient ratio create an advantage?
Let’s take a look at Medicare’s Public Use Files and examine the 10 percent who saved the most and 10 percent who lost the most:
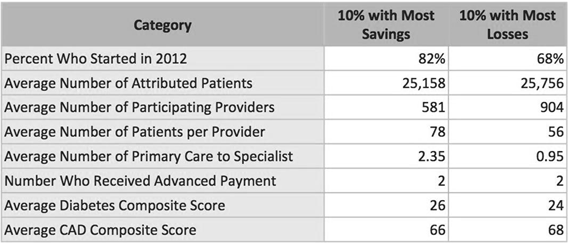
Common traits among the successful ACOs
• Have more experience, generally, although there are some exceptions
• The proportion of primary care providers to specialists is larger
• They have fewer providers but those providers have a larger patient load per provider
However, there are other attributes that are identical between the groups, leading to a couple of hypotheses for good research:
• The size of the patient population itself does not seem to determine success or failure
• Equivalent quality scores mean that higher resource use occurred in the Loss Group to reach the same results
• A number of factors may be at play to explain these hypotheses:
- Higher out-of-network traffic, with less patient outreach, loyalty or adequate referral decisions;
- Lack of coordinated care, leading to duplicate or higher cost tests and services;
- Improper attribution of patients to the ACO because of the primary-to-specialty imbalance.
• Network configuration is likely one of the most important factors to evaluate. The fact that losses occurred with higher provider counts and heavy specialty concentration points to the challenges for large multi-specialty and academic groups in ACOs.
Break the Barrier to Savings
There is no way to fake ACO success. The data shows savings goals can be reached, but it happens through careful design and implementation. Here are some of the main takeaways:
• Establish a performance measurement program that allows you to continuously evaluate outcomes and costs. The worst time to collect performance data is at reporting time because the data are subject to the arbitrary results of the patient sample and you can’t do anything about the results. The main purpose for performance measurement is not only to benchmark your providers and patient results, but also to identify patients and providers for focused interventions.
• Emphasize primary care when building your ACO network. Use CMS data to determine historical costs and quality profiles of all your network participants.
• Evaluate the cost and quality of specialists before you direct patients to them, as a best practice for establishing a referral network that will deliver both good outcomes and lower cost.
• Reach out to patients to foster patient loyalty and coordination of care and connect them with primary care providers in the network. There are several services, such as Medicare Wellness Visits, which are instrumental for this.
• Assess your ACO patient population attribution to ensure your patients have primaries in your network.
• Establish a Performance Improvement program built on interventions to the problems you diagnosed in performance measurement. After risk adjusting your population and benchmarking your data, the real work can begin—testing interventions and redesigning processes to bring the costs down.
Sources:
• Medicare ACOs Provide Improved Care While Slowing Cost Growth in 2014, CMS, 8-25-15
• Medicare ACOs Continue to Improve Quality of Care, Generate Shared Savings, CMS, 8-25-15
• Shared Savings Program Accountable Care Organizations (ACO) PUF, CMS, May 2015
The views, opinions and positions expressed within these guest posts are those of the author alone and do not represent those of Becker’s Hospital Review/Becker’s Healthcare. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them.
