(Hat tip to Emily Tchiblakian from Mercy Health who gave me this wonderful metaphor)
Before the internet, if you wanted to book a flight or hotel, you picked up the phone and called an agent. The internet changed all that. It gave you hundreds of websites and mobile applications to research options, read reviews and make reservations. In the next few years, you'll be picking up the phone and chatting with an agent again — but this time, you'll be talking to an AI-powered bot that will understand your needs and preferences, hunt down the best deal and take care of your reservations.
We're entering an era where machines will help us make sense of the vast amounts of information and get things done for us — bots, robots, assistants. We need them; we simply cannot deal with the information overload anymore.
Hospital leaders often ask: "We've spent tens of millions of dollars on an EHR implementation. On top of that, we have invested a lot on reporting capabilities; we have lots of dashboards throughout the hospital to keep track of everything. And teams of people dedicated to BI, reporting, data visualization, ETL and custom report generation. How can we leverage this investment to improve operational performance?"
And My Answer Is: Think Speedboats, Not Cruise Ships
EHRs are like cruise ships; they are large and slow to change "course" but have a lot of capabilities. EHRs have helped consolidate and rationalize the key pieces of data required to make better operational decisions but typically don't optimize or predict the future in meaningful ways. Similarly, dashboards and business intelligence tools have lots of good information and maintain meticulous records of every encounter, but they only generate historical views and provide just high-level direction, leaving the optimization challenge "as an exercise for the reader of the reports."
For example, in a key resource like the operating room, most health systems can track room and block utilization and drill down to individual surgeons to see their metrics: utilization, first-case on-time starts, turnover time, etc. However, making the metric visible isn't the same thing as improving on it. If a surgeon's block utilization is, say, 53 percent, what can we do about it? Can we take away 47 percent of their allocated time? No. Let's say, hypothetically, that we eliminated all first-case delays. Can we really reclaim those pockets of time and put cases in them? Not likely.
Everywhere we look, we have the data and periodic reports of current and past performance, but translating that data into actionable insight that improves operational performance in a sustainable manner is very difficult.
• Despite tons of monitors and metrics in the ER, patients end up waiting hours to get a bed. Of course, they get triaged within minutes after arrival, but they're frustrated with the endless waiting every step of the way — from admission, to operating room, to recovery, to discharge.
• Despite comprehensive metrics in operating rooms, blocks are often abandoned or underutilized while new surgeons struggle to find the block time they need to establish a viable practice. It can take weeks, if not months, to make block schedule changes.
• Many scarce assets in the hospital — imaging, clinics, labs — experience long patient wait times while simultaneously reporting underutilization of the asset.
What health systems really need are "speedboats" — specific, high-value analytical tools that go beyond dashboards and alerts. They place the right analytics, insights and recommendations in front of the right users (surgeons, schedulers, nurses and executive teams) at the right time through simple mobile and web tools. Physicians and nurses don't want to spend time on their desktops adding information and pulling reports. They want to spend time with patients. Technology has given them smartphones — now you can deliver the right information at the right time to make decisions that lead to superior operational performance and patient care.
Building Speedboats
The first step to building these speedboats is to create sophisticated predictive models to anticipate the volume, mix and timing of patient arrivals for today, tomorrow and the next several days. Then, it requires optimizing the allocation of the resources to match the operational constraints (assets, staff, skills) to deliver the smoothest patient flow possible. Since hospitals operate in an environment of extremely high variability, optimizations on paper will never suffice — they need to be run through millions of permutations and combinations of potential delays in sophisticated simulation algorithms to build schedules that are resilient to the inevitable delays that will occur. Finally, they have to incorporate machine learning to continuously compare the actual-versus-expected operational performance to identify the areas where a small adjustment will have a big impact.
There is no point in wasting the skills and talents of providers and their staffs to optimize a scheduling template or to anticipate bottlenecks building up in one or more care process. Their skills are better served in giving patients the best clinical care possible while leaving the data-intensive optimization to an intelligent machine. Technologies to make sense of data — natural language processing, image recognition, predictive analytics and machine learning, to name a few — have become advanced, mature and practical. They can help us make sense of data and give us actionable intelligence. This is no different than the way pilots of an intercontinental flight put the plane on autopilot as soon as it reaches a cruising altitude. The aircraft monitors hundreds of sensors continuously and makes dozens of micro-adjustments in the flaps, the ailerons and engine thrust each second, thereby delivering a more stable flying experience for passengers. Even the most skilled pilot could not possibly process all of that data and make all of the necessary adjustments every few seconds. Their human judgment is indispensable for unusual or emergency conditions, while leaving the routine micro-adjustments to an intelligent machine.
Speedboats are AI-Powered, Mobile-Delivered
The next generation of business intelligence will come from sophisticated algorithms that delve deep into data, understand patterns and provide actionable intelligence to the right individual at the right time. Algorithms will sift through reams of data to uncover insights we've not seen before. Machine learning will help providers understand patterns, make predictions and continuously refine their learning. Seamless and secure mobile experiences will send intelligent alerts, answer questions and help people be proactive and productive.
The best part is that these experiences will seamlessly work with existing data warehouses and other sources; all of the current investments will automatically be protected. Accuracy remains one of the biggest questions. On the clinical side, providers need an accuracy level that approaches perfection, but on the operational side, they can move the needle quite a bit — even with only 80 percent accuracy. This is the most important thing to keep in mind when providers think about taking their business intelligence to the next level.
It's Already Happening – Some Examples
1. "Open Table" for OR Blocks – Mobile Alerts for Block Releases and One-Click Block Requests: Most hospitals have OR committees that try their best to fairly and equitably allocate blocks to the right surgeons on the right day of the week. However, no matter how good the allocation, when reality hits, the best-laid plans become obsolete because surgeons are not able to use blocks (e.g., not enough cases, on vacation, clinic schedule, conferences, etc.), while others have a large backlog of cases for which they wish they had block time. Result: underutilized block time for some and others who could have used that time instead having a large backlog of cases each day.
Now imagine a simple Open Table-like tool that allows surgeons and their staffs to release blocks they won't be able to use or request vacant blocks they could use from a master scheduling process with one click. And what if this tool could also predict with high confidence and send proactive reminders to surgeons whose blocks look like they will go underutilized, encouraging them to release those blocks before the automatic release function?
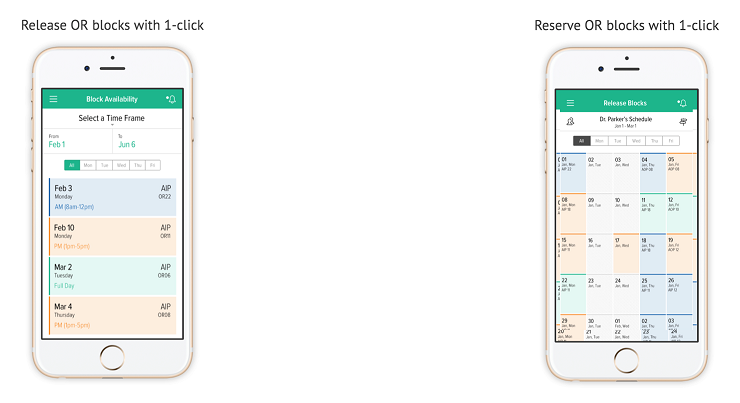
Huge efficiency gains — on the order of $250-500K per OR per year — can be achieved through this tool alone.
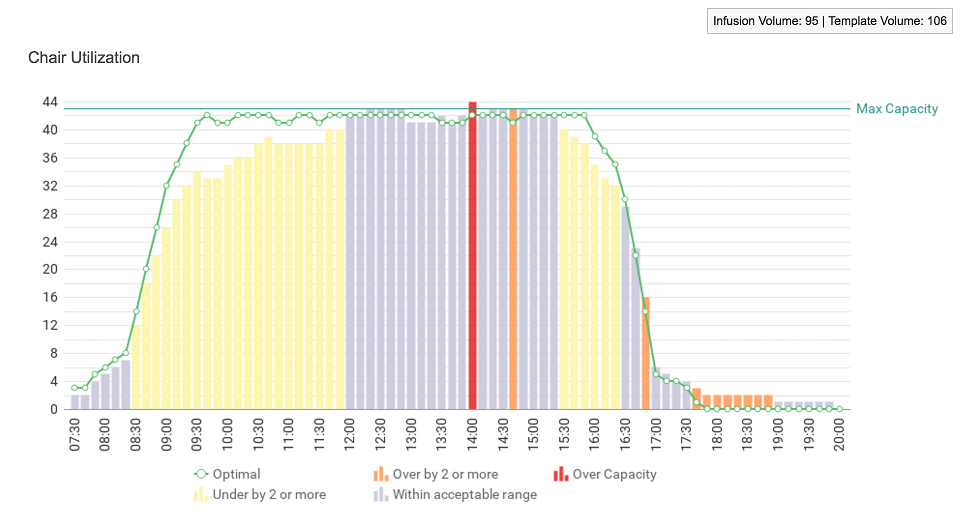
2. Slashing Infusion Center 10 a.m. to 2 p.m. Wait Times: Very few people realize that infusion scheduling is an extremely complex mathematical problem. Even for a 30-chair center, avoiding the 10 a.m. to 2 p.m. "rush hour" in a patient-centric way requires picking one of a Googol of solutions (yes that's 10 to the power of 100). But even with optimized schedule templates , an infusion center's ground-level reality — with last-minute add-ons that clinics send their way and late cancellations — means that what centers need are simple-to-use but sophisticated, mathematically optimized applications that send a "daily huddle report" each morning which lets nurses and infusion staff make fact-based decisions such as:
• What time of day is best to steer add-ons? When should nurses not take unscheduled breaks?
• How can the workload be fairly and evenly spread across nurses?
3. Emergency Room Streamlining: If the ED has 50 people waiting, how can timely, actionable information help identify which bottleneck needs to be resolved to clear the backlog? Is it because patients haven't been seen yet? Is it because patients are waiting for lab results? Is it because the imaging department is backed up or the lab understaffed? If a new patient needs an X-ray and a blood draw, should she be sent to the lab first or the imaging department?
Now imagine this: What if your ED director and staff had this easily accessible mobile browser application that showed them:
• Each patient's journey and how long each had been waiting
• The current, exact wait time for each device/department and what the wait times were for the last 30, 60 or 90 days
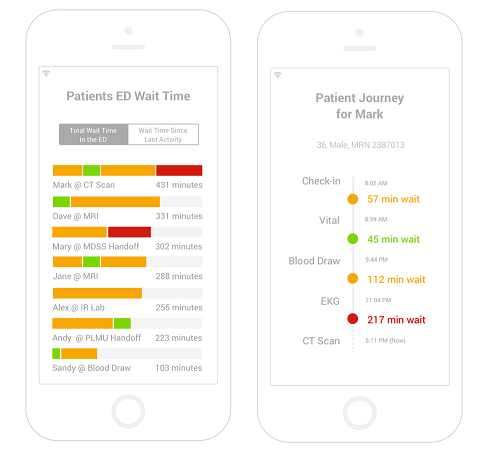

Now providers can see in real time how many patients are waiting for EKG results and where the backlogs are and then call for more staff and/or reroute patient traffic as much as possible to the less busy departments. More importantly, providers can fix the Wednesday staffing crunch at the EKG that repeats itself week after week because they have real data upon which to reroute traffic.
4. Accelerated Discharge Planning: What if case managers and social workers didn't have to work on everybody occupying a bed but instead could focus on a select few who are likely to be delayed in discharge? The EHR or some internal system is gathering "avoidable discharge delays" — who in the last month/quarter/year was delayed because of insurance verification, transportation unavailability, not having a place to go to, or nursing home/post care availability. If a provider has this data, it is a gold mine. What if it was possible that, within an hour of a patient coming in and filling out their forms, a provider could predict with a fairly high degree of accuracy who among their hundreds of patients is most likely (10-15 percent, if that) to be delayed in their discharge process? Case managers and social workers could have a much shorter list of high-priority patients whose discharge planning can start very soon after they are actually admitted.
5. ED to Inpatient Bed Transfer: How soon after a patient walks into an ED can the attending physician tell if they will need to be admitted? How many phone calls between the hospitalist and the ED physician does it take to board a patient? Is the data for each bed and its status available somewhere in a bed board? Do providers know, by unit, which patient's condition is well enough that they could be moved to a discharge lounge or are going through the discharge process? If all of this knowledge that already exists in the EMR, in the bed boards, or in the physician's mind could be combined, processed and analyzed in real time and exposed through a mobile browser-based tool, both the attending physician and the hospitalist could make decisions on the fly:
• Based on a patient's condition, provide an immediate estimate of which unit or units to which they could be routed.
• Get a set of options and agree on a likely onboarding flight path that is visible to everyone across the onboarding chain and upon which decisions could be made.
• Prioritize/dictate which beds should be cleaned first, which units should accelerate discharge and which patients should be moved to a discharge lounge.
An estimated 20-25 percent of healthcare cost is driven by the inherent challenge of making excellent operational decisions consistently, hundreds of times, day after day. Complex, multinode service processes that deliver a successful, safe outcome hundreds (or thousands) of times per day need to be built so that each node is correctly sized and has the ability to make excellent, near real-time decisions in an independent manner while leaving the overall choreography to a "master service process." This is how an airline can turn a plane at a gate within 40 minutes thousands of times per day in hundreds of locations. During those 40 minutes, an enormous amount of baggage is unloaded and reloaded, the tanks are refueled, the engines and tires checked, the food replaced, the cabins cleaned, crews swapped and hundreds of passengers taken off and reboarded onto the aircraft. Each of these subprocesses proceeded independently with full awareness of the deadlines involved; they made sure that they had the capacity (equipment and people) to deliver their part of the process. Importantly, all of this was done with hardly any artificial actions taken to expedite any of the subprocesses or to force any unnatural levels of coordination.
Hospital operations, too, have dozens of semi-independent subprocesses such as labs, imaging, clinics, infusion, radiation oncology, etc. that need to be coordinated to provide the care necessary for hundreds of patients each day. With predictive analytics performed in the cloud and used to send the right signals to the right decision-maker at the right time through simple-to-use web and mobile experiences, hospitals can maximize the enormous amount that they have already invested in infrastructure, EHRs and tools.
###
Sanjeev Agrawal is president and chief marketing officer of LeanTaaS iQueue. Sanjeev was Google's first head of product marketing. Since then, he has had leadership roles at three successful startups: CEO of Aloqa, a mobile push platform (acquired by Motorola); VP Product and Marketing at Tellme Networks (acquired by Microsoft); and as the founding CEO of Collegefeed (acquired by AfterCollege). Sanjeev graduated Phi Beta Kappa with an EECS degree from MIT and along the way spent time at McKinsey & Co. and Cisco Systems. He is an avid squash player and has been named by Becker's Hospital Review as one of the top entrepreneurs innovating in healthcare.
The views, opinions and positions expressed within these guest posts are those of the author alone and do not represent those of Becker's Hospital Review/Becker's Healthcare. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them.
