CEOs and senior executives also struggle to ensure that the board’s time and attention maintain this focus, appreciating that the oversight required of health systems today adds another critical layer of responsibility and accountability.
The relationship between trustees and healthcare leaders – premised not only on shared goals, but also on sufficient distance to promote objectivity of board members – continues to be a challenge, especially when it comes to oversight of healthcare quality. While a board’s time commitment to and prioritization of quality have been correlated with better performance on key quality outcomes on a hospital level, published research indicates that healthcare quality is still not sufficiently prioritized in board education and on board meeting agendas. Trustees often are more comfortable discussing and overseeing areas such as finance and strategy.
Trustees not only struggle to prioritize quality amidst a full board agenda and limited time, but also with how to understand the quality oversight they should do. IHI research, which included more than 60 interviews with thought leaders in governance education, representatives of state hospital associations, board leaders and health system leaders, found that boards are increasingly devoting time to overseeing quality but aren’t confident they are doing the right work. What are the correct areas to cover? What do leading boards do to oversee quality? How much time should be spent on one quality topic versus another? What questions should trustees direct to clinical leaders who bear responsibility for each area of quality?
Basketball coach John Wooden famously said, “Never mistake activity for achievement,” and this adage holds true in the boardroom. Many boards would benefit from a reliable way to align their quality oversight with best practices and from a clear understanding of how their governance is linked with organizational quality outcomes. So, where to begin?
Understanding variation in board oversight of quality
The Lucian Leape Institute (LLI), an initiative of IHI, recently completed a major study to understand the variation in guidance and practice driving board oversight of quality. This ambitious deep dive found that oversight of quality, especially the dimensions beyond safety, is highly variable and often not a board priority. Identified were three primary manifestations of this variability:
1. Quality is often not a board priority or area of competency.
Often, health system leaders do not establish quality as a board priority; instead, it falls to the end of the agenda or is brushed by as a quick approval item and is not always included in key performance measures of the health system. In addition, during our interviews board members regularly mentioned they are not as confident with their grasp of the concepts of quality as they are with other topics, such as finance, and are, therefore, often not as equipped or motivated for oversight in this area.
2. Guidance for health system boards is inconsistent.
Quality oversight guidance varies depending on which board education program trustees attend, their internal quality education efforts for trustees and which resources are shared for ongoing education. There is no standard of what should or should not be considered when governing quality making it difficult for trustees and those who support them to know they are on the right course for oversight.
3. The scope of the term “quality” has expanded faster than the corresponding oversight.
Health system leaders and trustees admit that they’re not up to speed with the expansion of the definition of quality from safety to a broader range of concepts, including care delivered across the continuum (beyond the walls of the hospital – in outpatient settings and in the community) and the health of populations.
While boards face system-specific challenges and considerations, we believe that certain universal oversight processes should be undertaken to effectively govern quality.
Building a new roadmap for governing quality
Driven by a concern about the variation in board oversight of quality, IHI’s LLI decided to develop a new resource to address this challenge and convened a group of experts to build a new roadmap for governance of quality. Participants included leading health system CEOs and senior leaders and representatives of forward-thinking organizations, such as the American Hospital Association, American College of Healthcare Executives, The Governance Institute and state hospital associations. Through a collaborative process, LLI built a new framework for governance of quality that is outlined in the IHI report: Framework for Effective Board Governance of Health System Quality.
The framework identifies three core areas essential to quality oversight for trustees:
• Prioritization of and commitment to quality;
• Understanding of the organization’s system of improvement; and
• Understanding of core quality concepts across all the dimensions of quality.
The report identifies the core work for governance of quality and provides concrete guidance documents with ideas for each of these areas to help trustees and senior leaders support their boards.
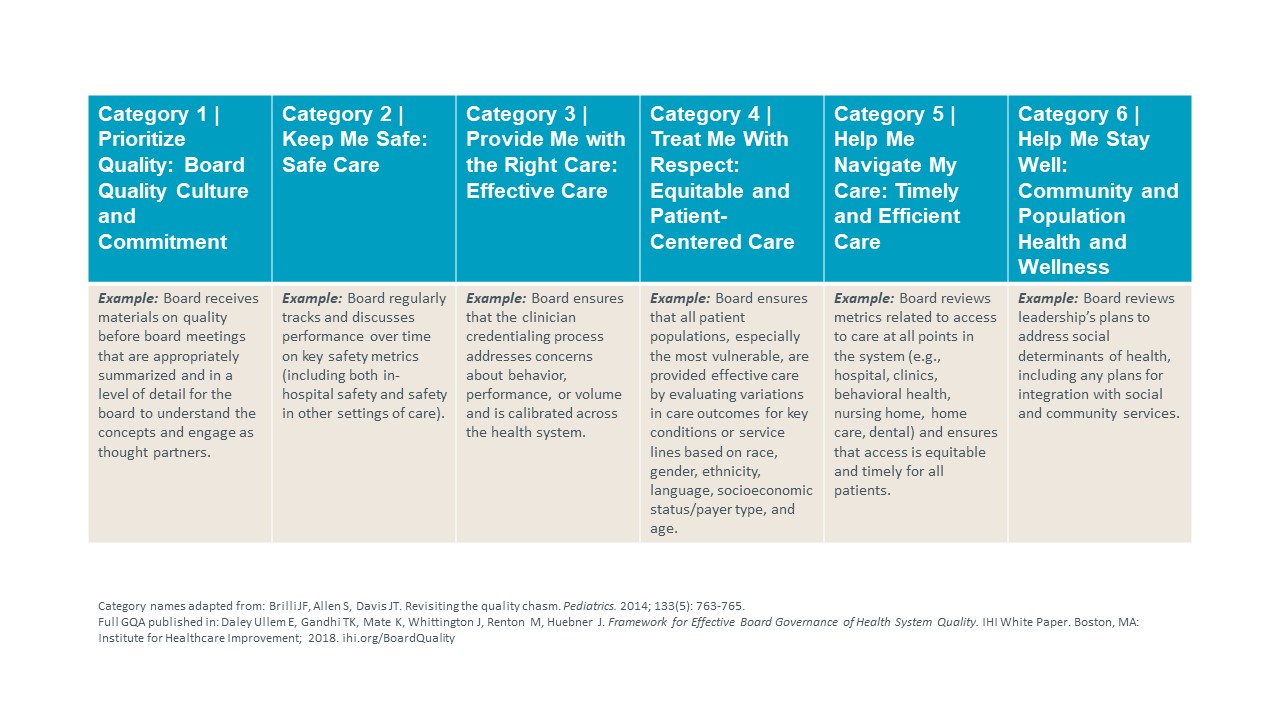
To supplement this guidance, IHI’s LLI built an online assessment tool, The Governance of Quality Assessment (GQA). It evaluates 30 core processes deemed important for excellence in quality oversight. Each health system can decide, based on its unique structure, the processes that should be governed at the level of the health system, board quality committee or individual hospitals or business divisions. Notably, the GQA incorporates the six dimensions of quality identified by the Institute of Medicine in Crossing the Quality Chasm: care that is safe, timely, effective, efficient, equitable and patient-centered. The GQA also includes population health and board culture of quality.
Governance of Quality Assessment (GQA) – Categories and Examples
Taking the next steps
IHI recommends that health system leaders, board members and board quality committee members complete the GQA to serve as a baseline measure and to foster discussion of the current state of board oversight of quality. After completing the GQA, they should ask these questions:
• What is the score for the GQA overall and for each of the six categories?
• Where are gaps that identify areas for better oversight?
• What area should be prioritized?
• Are there low-scoring areas that could be improved through education or greater understanding of the health system’s work?
• What specific actions can the board take to improve low-scoring areas?
The goal of the assessment is not to focus on a numeric score, but rather to facilitate discussion and accelerate quality oversight. The tool allows boards to easily track oversight processes over time and to compare their work with that of other boards to share ideas for improvement.
Calling healthcare to action
As healthcare becomes more complicated, quality oversight needs to do more and do better to accelerate and support quality care. Boards don’t do enough to oversee organizational quality along all dimensions. Boards can and should do better to oversee quality. They should understand the core oversight processes; assess the organization’s performance; and identify opportunities for improvement. Furthermore, boards should commit to thoughtful discussion and a culture that puts quality first, recognizing it as the essential element of an organization’s core product to deliver to patients.
Quality is a moral and financial imperative; it should be owned as the core of operational excellence. Better quality will reduce cost, improve outcomes and provide the workforce with a more healing place to come to work.
Healthcare leaders and trustees need to call their own organizations to action to dramatically accelerate and improve governance of quality.
