The response was strong at Riverside Medical Center, an acute care facility in Kankakee, Illinois, when a confluence of patient-care and cost-based issues came to a head several years ago. The 325-bed facility suddenly found itself staring down pressing challenges, including an increase in length of stay; a rise in denials; poor documentation; lost reimbursement dollars; and a general lack of preparedness to meet an evolving healthcare system
“It was pretty much the Wild West,” says David Duda, chief operating officer at Riverside. One of the biggest challenges Riverside faced was that the facility – and, more specifically, some of the staffing departments – were ill-equipped to deal with the external factors pressing in from all sides. Workflow and job responsibilities among case management, utilization review and bedside nurses were stuck – if not in the past, then in a mire of inefficiency.
“Their jobs were antiquated for all the rules and regulations that have come upon the hospital industry,” he says. “We were, like other hospitals at the time, feeling overwhelmed by these rule enforcements.”
This present-day perspective is borne out of hard-won experience. In late 2011, Riverside launched the initial steps of what proved to be a significant restructuring of its case management department. The facility sought an antidote to counteract its slipping quality measures and lost days, with the focus resting on three crucial words: Progression of care.
New roles for a changing ecosystem
The entire mechanism of change within the case management department at Riverside was built on a new way of thinking, a tactical decision to reformulate the way that case management operated in relation to other professionals, departments and patients.
Previously, Riverside had utilized a unit-based case management model, in which one professional was responsible for patient case management, utilization review and discharge planning. While an RN case manager is equipped to handle these various functions, the fact that they were all wrapped up into one job translated into lost opportunity – to stratify roles of the professional staff in order to meet an evolving market.
“The scope of hospital case management has changed drastically over the years,” says Stefani Daniels, RN, MSNA, CMAC, ACM, who consulted with Riverside as they redesigned their case management operations. “Now case management is looked to as a core function for maintaining quality care and improving the hospital’s bottom line.”
Through a subtle but transformational shift, Riverside remapped their case management department, doling out a new role to CM staff. The main crux of it was that the case managers would no longer be unit-based. Instead, case managers would affix themselves to physicians, and round with the doctors with one central end in mind – to facilitate the patient’s movement through the hospital.
“In our model, the case manager’s main objective is to progress the care of the patient – meaning that they deliver the right treatment in the right setting at the right time,” says Eileen Krach, Riverside’s director of care management.
While evolving reimbursement models contributed heavily to this new way of thinking, the acknowledged dangers of a hospital stay also form a paramount role. “We don’t want patients in the hospital longer than they need to be,” says Krach. “We know that hospitals are not the ideal place for patients to be.”
Dr. Stonewall McCuiston, medical director of clinical integration, agrees. “The longer you stay here in the hospital, the more likely something negative is going to happen,” says McCuiston.
That this adage reflects reimbursement policy is hardly a coincidence. Increasingly, payers are reimbursing providers for the value of their care, rather than volume. And metrics like length of stay and readmissions, along with quality-associated attributes like medical necessity, are pivotal areas of concern. The physician-based case management model targets these pressing concerns, and the new model, through which Riverside has gleaned substantial cost and quality improvements, means a dramatic change in the day-to-day work of the case management staff.
Where they once had their eyes glued to patient records, case managers now interface with patients in a much more direct way.
“You have to be rounding,” says Duda. Riverside’s case managers don’t look in the records anymore. Instead, they talk to the nurse taking care of the patient. They talk to the patient. They round with physicians when they go in to consult with a patient. All of their efforts are aimed at facilitating the patient’s progression of care.
By and large, physicians have been pleased with the change in protocol, says Dr. McCuiston, primarily because it “streamlines” communication channels between doctors and their support staff. “Before, you had a different person for each floor. Depending on how many floors you went to, that’s how many different people you’d have to talk to,” explains McCuiston. “Now you only have one case manager.”
Krach sees a tangible benefit from this streamlined communication. “The physicians appreciate it,” says Krach. “They like having a point person.”
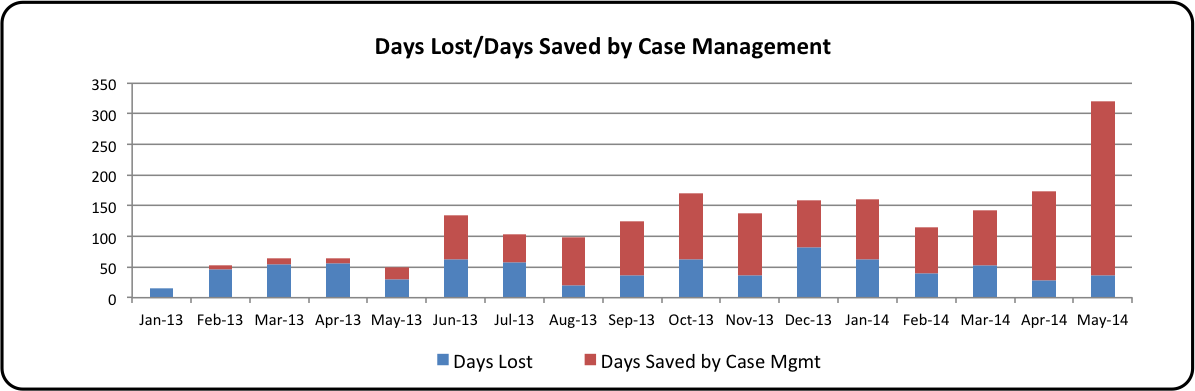
Team communication is not the only area where the hospital has seen a significant boost. Among other improvements include a host of quality metrics, from length of stay (see Table 1) to patient readmissions. What’s more, case mix index – that elusive, telltale number – has increased, proving that the hospital’s documentation is accurate and the decisions governing care delivery are well-founded. (See Table 2 for saved days attributed to case management.)
Defining progression of care
When viewed in an historical context, hospital case management is in a relatively early life cycle. It emerged in the 1980s as an outgrowth of the market shift from cost-based reimbursement to prospective payment models. It further evolved with the demands surrounding the booming managed care arena. As modern priorities again shift, healthcare leaders are realizing that case management programs must follow suit.
“We are seeing new demands placed on healthcare facilities, and as a result our models of care must adapt to meet these demands efficiently and effectively,” says Daniels, who consults with leading providers daily with her firm Phoenix Medical Management.
With a focus on outcomes, progression of care is designed to meet these evolving demands. The outcome model of case management is largely defined by:
– Redefined work structure. In the outcome model, case managers align themselves with physicians and join in daily/regular rounding. By attaching case managers to individual physicians, and thereby individual patients, the department’s ability to coordinate care gets a significant boost and case managers are better positioned to influence physician practice decisions. “If you have strong case managers, they can really help influence the progression of care with your patients,” says Krach.
– Separation of case management and utilization review. This point is elemental to the progression of care paradigm, and allows for focused attention to the patient’s care path on the one hand (via case managers), and compliance with payer policies regarding patient status and criteria for continued stay, among other variables (utilization review). Separating the job functions allows for greater efficiency in both areas. On one side, “we have case managers, whose job is to flex their schedule to match the schedule of the physicians who are rounding,” explains Duda. On the other are “designated UR staff, who have become the ‘go to’ experts on the rules governing utilization review.”
– Constant communication. Because the case manager takes on a more patient centered role, it is essential to maintain open lines of communication with physicians and other colleagues, according to Krach. Daily huddles that last between 10 and 15 minutes keep all parties connected with the patient’s movement throughout the facility. These daily meetings have proven to be a key way of maintaining appropriate documentation by allowing case managers and utilization review nurses to communicate and ensure patients meet criteria for a continued stay, testing, or movement elsewhere. A dedicated UR nurse brings much-needed expertise to the conversation. “With all of the contract negotiating with commercial insurance providers, you have to have staff who’s dedicated to knowing what those changes are, and having that rapport with case managers from commercial payers,” says Krach.
– Designate a nurse unit leader. Riverside found that designating a nurse leader in each unit to act as a go-to source for patient information is a significant efficiency booster. Instead of case managers chasing down an individual nurse for a question about a patient’s care, they can direct their questions to the designated point person and save time and energy in the process.
– Shuffle patient placement. While not a requirement for launching an outcome model, Riverside found it helpful to move the physical locations of their patients based on their status. All observation patients, for instance, reside in a dedicated clinical decision unit on the first floor, while other patients who have been admitted as inpatients are pooled together elsewhere.
Steps to implement change
When the leadership at Riverside set out to redesign its case management department, it met a number of challenges ranging from mapping out a sensible, comprehensive plan to resistance among entrenched staff. As the transition plan rolled out, staff members on both sides of the aisle – physicians and case managers alike – displayed signs of apprehension, confusion and ambivalence, says Duda. The message from the leadership suite had to be strong.
“The train’s going one way,” Duda recalls his message to staff. “You’re either on it or you’re not.”
In hindsight, the choice to move into the outcome/progression of care model makes perfect sense. Yet at the time of transition, when the established roles and job duties of long-time staff were in flux, there was no small amount of turbulence. The strength of their convictions, expressed in a roadmap, helped ensure the leadership team achieved staff buy-in, the correct processes for change, and, ultimately, the quality and financial dividends they aspired to.
The following best practices showcase the key elements of Riverside’s transition to a fully functional progression of care case management department.
– Identify priorities. It is imperative in today’s environment to focus staff efforts on quality and compliance, says Krach. It may be helpful to consider these questions: “Are we performing the right treatment in the right setting? How are we progressing care? Are we facilitating the discharge?” Answering these questions will help spot lapses in care that ultimately can lead to compromised outcomes and associated reimbursement levels.
– Bring in expert advisors. Given the complex stew of payer rules and regulations, the expertise of consultants can reap significant dividends, according to Duda, who worked with Daniels’ firm, Phoenix Medical Management, to carve out the process-of-change plan. The trained insight of consultants provided a clear view of the hospital’s challenges – and opportunities – that they otherwise would not have gained. In Riverside’s case, this began with a 50-page assessment of the hospital’s case management, utilization review and general progression of care challenges. It continued with key point-by-point guidance as the transition plan moved from theory to practice.
– Engage staff and leadership. “Getting people to change is going to be the hardest part,” says McCuiston. But he advises, “Don’t give up in the beginning.” While the change met some resistance among staff, resulting in approximately a 40 percent turnover in case management staff, according to Duda, it is vital to clearly define the plan of change, the elements that comprise it, and the important role of staff in the transformation. The big key, says Krach, is to “clarify and define expectations for your staff.”
– Reinforce, reinforce, reinforce. Any large-scale transition will cause ripples in the day-to-day work of staff, but maintaining a steadfast commitment to the plan will help smooth over the inevitable bumps along the road, according to Duda. This is true for the range of involved parties, from the hospital board all the way to the medical staff. “Without engaging them over and over again, I don’t think we would have been successful,” says Duda. To sustain staff commitment, share early successes and be sure to maintain open lines of communication between medical staff, leadership and other stakeholders.
– Spend early to achieve ROI. Progression of care involves revised staffing roles, and it may create the need for new staff positions altogether. As it transitioned to the new model, Riverside added seven additional full-time RN positions to fulfill the changing roles. As mentioned above, the dollars budgeted for outside consultants may be an additional cost, but one that sees a strong return on investment. “It sounds expensive,” says Duda. “But what we saved more than makes up for the investment.”
Table 1
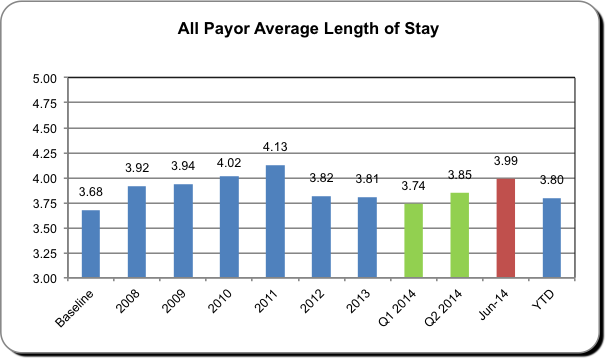
Table 2
The views, opinions and positions expressed within these guest posts are those of the author alone and do not represent those of Becker’s Healthcare/Becker’s Hospital Review. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them
