5 elements of building high-impact quality programs for anesthesia and pain management
Ask a group of anesthesiologists to give a business card to their patients and they might look at you like you have two heads. "You don't give them your private number do you?" Well actually, I do. Giving patients access to their providers is an important part of a Quality Program. If patients can't reach a real person on the other end of the line when they need help, we're no better than the cable company. Being accessible doesn't just make sense—it's the right thing to do.
But handing out business cards is just a small part of building a comprehensive Quality Program. As the concept of pay-for-performance continues to mature, there will be a corresponding emphasis on quality. Anesthesia and pain management practices can adjust to the new pressures by making sure their quality program contains the following components: vigorous data collection, a supportive organizational culture; continuous education and training; ownership of information and robust patient satisfaction measurements.
1. Data collection - Quality measures are nothing new in healthcare. They're now expanding beyond primary care with a renewed focus on better data gathering, prospective and predictive measurement and patient engagement. Metrics drawn from this data create a continuous information loop that helps propel quality efforts and improve the satisfaction of our payers, healthcare systems, facility administrators, stakeholders and patients. Yet while data collection provides the means for building a quality program, it is not an end in itself.
2. A culture focused on quality - Top-notch technology and data collection will not advance a Quality Program if the process that it supports is not clear and valued by every provider. An effective Quality Program creates a culture that encourages and rewards the reporting of critical incidents, identification and pursuit of best practices, and continuous process improvement. Most importantly, the organizational structure must support this culture of quality from the top down.
3. Education and Training - Providers should be continually involved, educated and trained to build quality into everything they do. There must be dynamic two-way communication between a central Quality Program and each practice location. Designation of a physician and/or CRNA at each practice location to be responsible for this two-way communication is essential. Effective education and training includes
- Creating a culture of reporting
- Identification and pursuit of best practices and continuous process improvement
- Continual feedback on all measurable quality activity
4. Own Your Information - Anesthesia practices are well advised to own their own data in order to better manage and control it. An EHR or anesthesia information management system (AIMS) allows effective capture of a wealth of digital data, but data collection must also come from partner hospitals, payers and patients. Collecting digital data from a variety of sources adds a level of technical complexity and requires professional information management, but can reap significant benefits.
"Owning the Information" also requires robust in-house data warehousing, analytics and reporting capabilities. As a management tool this is critical, and with hospitals now taking "at risk" contracts, having their anesthesia provider tracking and delivering reliable metrics can be very beneficial to the hospital-practice relationship. As an organization, being able to report on what you want, when you want, is powerful.
5. Effective Measurement of Patient Satisfaction - Patient satisfaction is an important outcome of a successful quality program and validation of the effort. Like clinical and demographic data, patient satisfaction needs to be measured and reviewed to identify areas of improvement.
Technology can also support this objective through an electronic anesthesia patient survey system with feedback via alerts, detailed reports, audio and text comments and individual interventions.
PhyMed practices use SurveyVitalsTM Anesthesia Patient Survey Questionnaire (APSQ) to survey patient experience. Some recent results from these efforts show very positive impact.
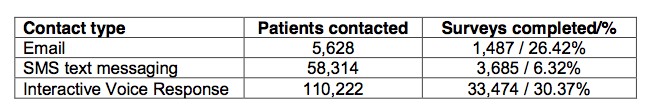
The 25% patient response rate to the APSQ handily exceeds the industry standard, and less than 4% have opted out. Survey information is made available to practices through online portals that can be accessed at the organizational and individual practitioner levels. These post-op surveys were also timed appropriately according to the surgical outcome.
As part of our survey process, one hip replacement patient, contacted a week following her surgery responded: "I rarely respond to surveys requesting customer feedback, but the survey was something I wanted to do. I had a terrific outcome, but if it helps make the next patient's surgery go that much smoother, it's worth the time."
The survey also found that simply asking patients about their experience—good or bad—improved satisfaction levels.
Low scores on the APSQ generate alerts to administrators and practitioners so problems can be quickly addressed. Measuring the patient experience in this way, together with the capability to "close the loop" with practitioners and staff has led to measurable improvement in overall patient satisfaction scores. And that's good news all around, as private liability insurance companies have noted the correlation between high patient satisfaction scores and a lower incidence of medical malpractice suits.
A robust Quality Program gives providers the ability to move quickly in any direction in terms of outcomes measurement, reimbursement and compliance with new government standards. And for providers, bending with the winds of change in healthcare is the key to short and long-term success
1 Sanford, J.A., Macario, A. 2014. Data, data, on the Server. Anesthesiology 121 (1); 6-8.
2 Measuring Anesthesia Patient Experience – APSQ Study Abstract
3 Stelfox, H.T., Gandhi, T.K., Orav, E.J., & Gustafson, M.L. 2005. The relation of patient satisfaction with complaints against physicians and malpractice lawsuits. American Journal of Medicine. 118:1126-33.
4 Saxton, J.W., Finkelstein, M.M., Bavin, S.A., Stawiski, S. 2008. Reduce Liability Risk by Improving Patient Satisfaction. Press Ganey Associates, Inc., July.
The views, opinions and positions expressed within these guest posts are those of the author alone and do not represent those of Becker's Hospital Review/Becker's Healthcare. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them.

