One mission of CMS is to ensure that patients admitted to the hospital receive proper care from their physicians as well as an effective discharge plan. The idea is that if patients leave with a future-care plan in place, they will not walk back through hospital doors days or weeks later. Better partnerships between hospitals, payer organizations and outpatient provider groups (local visiting nurse associations, for example), from the point of admission, during the time of care, through to discharge and post-discharge care coordination could significantly help many hospitals address and reduce 30-day readmission rates.
CMS recently announced that hospitals readmitting patients within 30-days of discharge will be hit with a 3 percent fine to their Medicare payments in fiscal 2015 as an effort to reduce excessive amounts of readmissions. This represents a 1 percent increase from 2014.
According to 2013 findings from CMS Research on Medicare, nearly 18 percent of Medicare patients who had been hospitalized were readmitted within one month. While that is lower than past years, roughly 2 million patients return each year, costing Medicare $26 billion. Officials estimate $17 billion of that comes from potentially avoidable readmissions. This is exacerbated due to the lag of readmission data that is reliant upon the processing of Medicare claims, which can take up to 13 months for a claim to reach "final action" status.
Real-time clinical intelligence and collaborative care for prevention of avoidable readmissions
Some of the other methods that CMS has taken to lead the national effort in the reduction of readmission among its most vulnerable patient populations are:
- Hospital Readmissions Reduction Program
- Partnership for Patients
- Shared Savings Program
- Quality Improvement Organizations
However, based on the CMS 2013 report, it is the extremely latent readmission data feeds from Medicare claims data for Part A beneficiaries, with no risk adjustment applied, which CMS relies upon to retrospectively track and implement fine-based interventions to hospitals and to provide a primary motivation for change in discharge protocols related to poor care outcomes. This issue is endemic across all payer organizations — the inability to receive and be alerted of high risk patient populations' admission, transfer and discharge status at the time of care, for meaningful intervention with their provider networks.
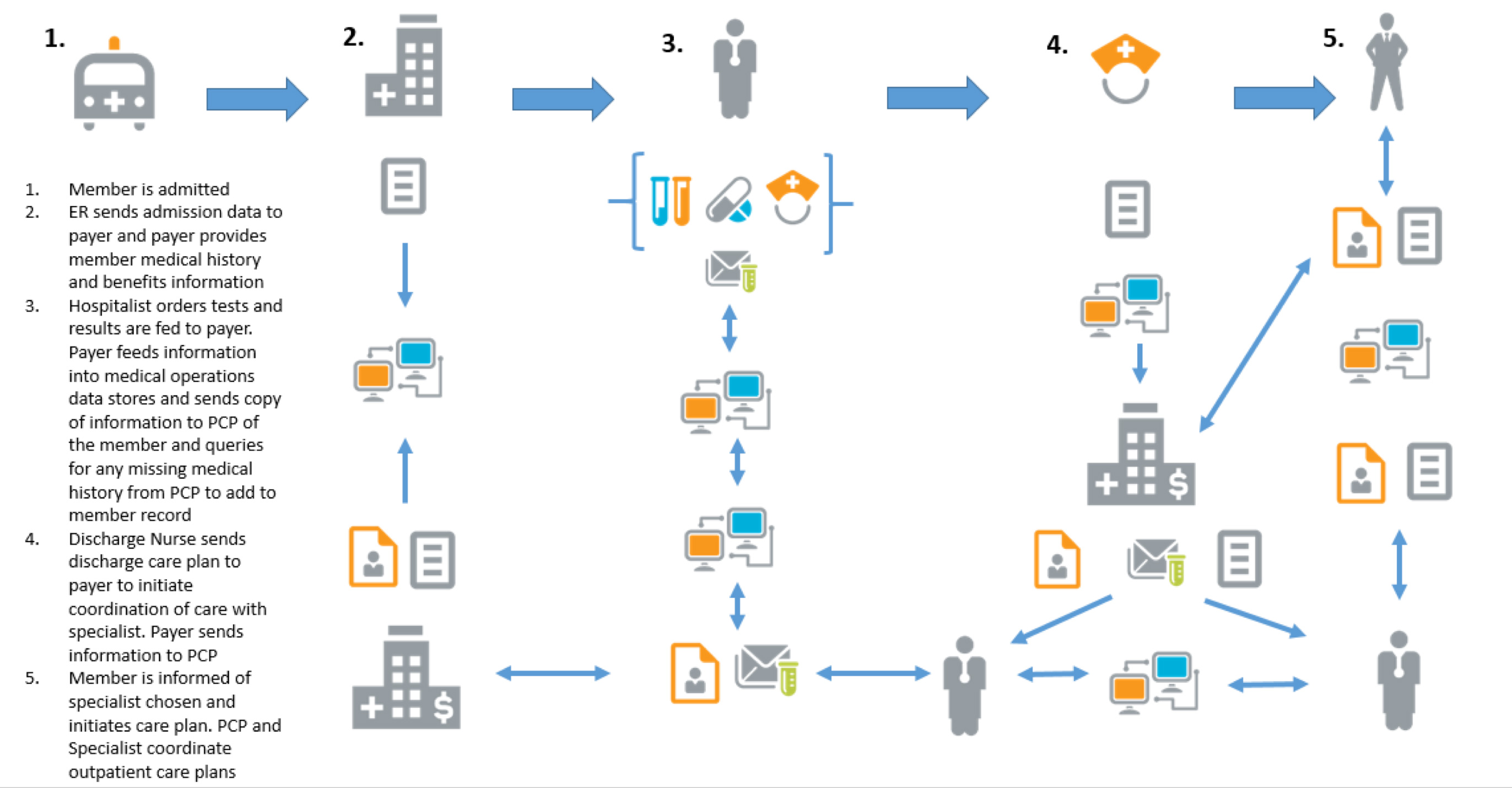
The ideal situation is for the provider and payer to share the status of the patient and the patient's medical history at the time of care in order to mitigate the risk of a readmission event before the admission event takes place. There have been great strides in both the private and public healthcare sectors to address this chronic issue; new and innovative healthcare information technology and collaborative care models, such as accountable care organizations and patient-centered medical homes, are emerging as proven solutions designed to address the disparities in timely clinical intelligence between providers and payers to prevent avoidable readmission events. One such healthcare technology standard is HL-7, a data exchange standard that is not only endorsed by the Department of Health and Human Services ONC for meaningful use incentive programs for its Medicare providers, but is also a trend private payers are adopting as a means for addressing this patient safety and quality of care issue. An example of how HL-7 is used is illustrated in the diagram below:
As part of the HITECH legislation, incentive programs related to the deployment of EMR systems that have the HL-7 clinical data exchange capability were supported and adopted, but not with the significant growth that was anticipated. The cost of procuring and maintaining these systems, as well as adjusting to the initial workflow disruption, has limited the national impact it was intended to have. In spite of the growing pains of adoption, providers and payers alike see the value of these health IT investments and understand how they contribute to the improvement in care outcomes related to discharge planning.
During the peak of the HITECH legislation rollout, both federal and state health agencies also endorsed the development and adoption of public and private health information exchange networks, such as regional health information organizations. At the national level, there has been limited success in providing a widespread, financially sustainable public HIE network for real-time data exchange across healthcare communities. However, there are examples of adoption in some states including California, New York and Maryland, with measurable impact to care coordination and improved patient safety.
An October 2013 report commissioned by HHS' Assistant Secretary for Planning and Evaluation Office of Disability, Aging and Long-Term Care Policy revealed that long-term and post-acute care providers with very effective HIEs in place experienced the exchange of timely admission and discharge data resulting in opportunities for both providers and payers to proactively mitigate readmission of high risk patient populations with collaborative care models, such as ACOs and PCMHs.
The adoption of EMRs and/or HIEs that enable real-time patient-level data exchange between providers and payers, within the context of collaborative care models, have been shown to provide actionable intelligence by the healthcare community to stem the tide of readmission growth trends.
Pre-admission and post-discharge care coordination
Some of the root causes of the avoidable readmission penalties result from inconsistencies in ER care management protocols. There is a higher rate of success if the patient is accurately diagnosed and treated fully while in the ER and/or a proceeding inpatient stay, before being discharged for certain disease states that outpatient care teams cannot address. There are some key HEDIS and disease management protocols that, if not followed in route to and addressed fully in the ER (for example, a stroke victim), the patient's care outcome for a successful discharge will be unlikely, due to this avoidable domino-effect with readmission. This has led many hospital-based quality managers to utilize alternative quality assurance methods, such as Six Sigma and lean principles, to perform more effective root cause analysis and re-evaluate and re-engineer faulty clinical and operational protocols to stem the flow of readmissions at the point of care.
From a discharge planning perspective, hospitals can prevent many avoidable 30-day readmission instances by leveraging the services of visiting nurses, long-term care coordinators and patient advocate service providers, some of which may be supported by authorized case management programs from private and public payers as part of the discharge care plan process. This is contingent upon the payer community providing hospital staff at the time of discharge and obtaining timely eligibility and benefit information that align to the patient's insurance coverage and compliment the prescribed discharge plan. This approach to coordination of care at the time of discharge should also provide real-time information to the patient's primary care physician (see diagram above, which illustrates this). Coordination such as this is regularly practiced in ACOs and PCMHs in order to meet the standards of care associated with these collaborative care models.
Defensive medicine tactics and high-risk patient population groups
Not all patient populations are equal, nor do all have access to the same healthcare resources as fully insured, low-risk patient groups. As a result, there is also the opposite effect of the use of defensive medicine tactics for some hospitals, such as safety-net hospitals. Oftentimes these organizations that suffer a recurring pattern of readmissions from their high-risk patient population groups respond by either admitting patients where there is no cause for admission or keep return patients in a broken loop of high-cost specialty care in order to prevent revenue loss due to fines. This is where programs such as CMS' Partnerships for Patients can be applied to high-risk patient populations in extreme socio-economic hardship settings, to give safety-net hospitals a viable solution for minimizing the rising cost associated with care management within this community of patients.
The National Quality Forum has also recommended a re-evaluation of the appropriateness of readmission measures identified by CMS for safety-net hospitals due to the unique socio-economic challenges that different patient populations face, according to a published statement from Kaiser Health News. In addition to implementing community-specific readmission prevention programs, it is critical that these hospitals have access to reliable clinical intelligence and shared population risk stratification reporting among their public and private payer partners for effective care management. This can be achieved through a partnership of real-time data sharing agreements across provider, payer and public health agencies at large.
If we raise the priority for adopting real-time clinical intelligence at the time of care, support transparency and trust between the patient, provider and payer related to post-discharge care options in a collaborative care delivery system, the U.S. healthcare system will begin to significantly reverse the trend in avoidable readmission rates among our most vulnerable patient populations.
The views, opinions and positions expressed within these guest posts are those of the author alone and do not represent those of Becker's Hospital Review/Becker's Healthcare. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them.
