Many healthcare leaders are strategizing to meet the requirements of section3022 of the Patient Protection and Affordable Care Act. This historic passage of legislation to reform our nation’s healthcare is requiring new thinking and action. Although many of the specifics of the reform act are not yet defined, healthcare organizations can be proactive and strategically position themselves for success. With expected reimbursement decreased by 20-25 percent, new systems and networks will be developed between providers. The first step is for leaders to become educated on what is known about Accountable Care Organizations and then assess where their organization is in relation to the known requirements.
Building a Roadmap to Readiness
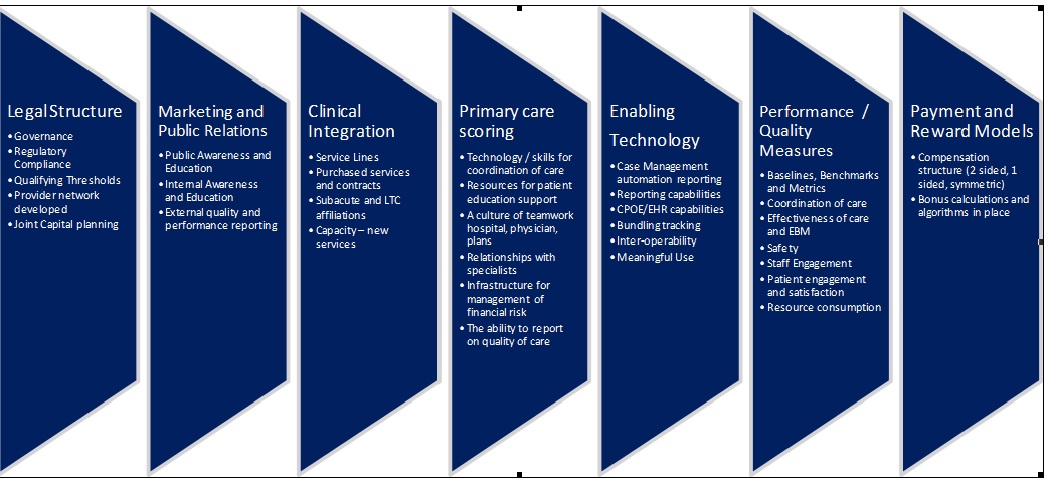
A readiness assessment process is necessary to aid healthcare organizations in comprehensively evaluating their strengths and priorities as they progress toward accountable care. This is one approach that identifies seven assessment categories that are critical to address for success in today’s market. This process can help organizations meet their current challenges and develop a roadmap for building a higher performing organization. An Accountable Care Organization should be centered on providing an excellent patient experience, and it should produce outcomes that indicate they are controlling costs, and improving quality. The assessment must address these areas and more. There is no doubt that this is work already in progress in many organizations but the difference is the shift in accountability to be assumed in new partnerships between physicians and hospitals. The goal is to build on the good work in progress and target the high priority areas for change.
Assessment Approach
A formula for success includes an experienced leadership team using analytical tools and data to comprehensively look at the current processes and outcomes related to creating a successful environment of Accountable Care. Through the use of technology it is possible to identify clinical variations and opportunities to reduce resource consumption and increase throughput in the organization. Physician-driven collaboration with the hospital is key to maintaining hospitals' profitability through clinical cost containment while minimizing the potential of compromising care. Using physician-directed process improvements, the hospital can make data-driven decisions that reduce the use of hospital resources, obviate costly errors and control variations in care delivery that compromise medical outcomes.
Assessment Components
In this process there are over 300 key checkpoints critical to understanding the level of preparedness for each of the seven assessment categories. Each of the 300 indicators can be reviewed, weighted and scored numerically to gauge readiness. In addition to the clinical performance data, the approach should include web-based surveys, data requests, workshops/interviews, capacity mapping and process reviews to identify both operational and strategic actions required to move forward with a coordinated care delivery model design.
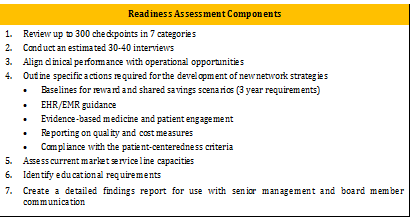
Readiness Assessment Components
1. Review up to 300 checkpoints in seven categories
2. Conduct an estimated 30-40 interviews
3. Align clinical performance with operational opportunities
4. Outline specific actions required for the development of new network strategies
6. Identify educational requirements
7. Create a detailed findings report for use with senior management and board member communication
(Right click on image for a larger view)
Weeks 1-2
The initial weeks are a time to do a behind-the-scenes review of operations and data within the seven areas of readiness. The internal and external stakeholders should be identified for involvement in the assessment. A series of interviews can be conducted with key senior leadership and other professionals identified. The interviews focus on questions that align with the seven areas of accountable care priorities as well. These interviews will be designed to uncover a broad understanding of the hospital and physician general operations and integration. The interviews will also serve to enhance communication, build relationships and identify concerns. The strengths and weaknesses of clinical coordination and integration can be determined and the initial opportunities for enhancements identified. A technical assessment should be done of the quality and cost data. This assessment will identify variations in delivery of care and consumption of resources
Weeks 3-4
During these weeks, the data and information collected can be collated and analyzed. This includes scoring of all the check points within the seven areas. The scoring system can help identify the lower areas that need to be progressed to full readiness. Once the full picture is revealed, the leadership team can begin outlining actions required to maintain areas of high effectiveness and address areas of low readiness. This calls for discussion and dialogue to create innovative approaches to move forward.
Weeks 5-6
Presentations of identified findings and opportunities to validate them with can be made to stakeholders and generate additional ideas and input. There may also have been some educational needs related to accountable care identified for key groups or individuals that can be delivered in conjunction with the organizational results.
The leadership team and identified stakeholders can use the results to build scenarios and create new possibilities to achieve desired outcomes. The readiness assessment is the basis for the continued planning and action. As new information becomes available the leadership team must have the capacity to be flexible and adjust to new information and circumstances. Readiness assessment findings will assist healthcare leaders in making informed decisions and developing focused strategies as healthcare regulatory change begins in 2011. A comprehensive approach such as this one, is necessary if healthcare organizations want to not only “Survive but Thrive” through healthcare reform.
Learn more about Verras Consulting.
Building a Roadmap to Readiness
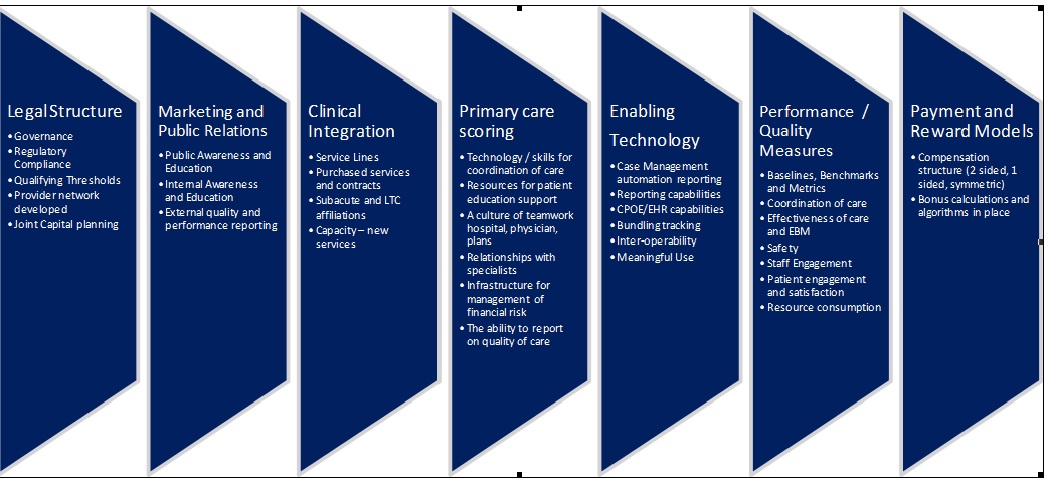
A readiness assessment process is necessary to aid healthcare organizations in comprehensively evaluating their strengths and priorities as they progress toward accountable care. This is one approach that identifies seven assessment categories that are critical to address for success in today’s market. This process can help organizations meet their current challenges and develop a roadmap for building a higher performing organization. An Accountable Care Organization should be centered on providing an excellent patient experience, and it should produce outcomes that indicate they are controlling costs, and improving quality. The assessment must address these areas and more. There is no doubt that this is work already in progress in many organizations but the difference is the shift in accountability to be assumed in new partnerships between physicians and hospitals. The goal is to build on the good work in progress and target the high priority areas for change.
Seven Assessment Categories
Assessment Approach
A formula for success includes an experienced leadership team using analytical tools and data to comprehensively look at the current processes and outcomes related to creating a successful environment of Accountable Care. Through the use of technology it is possible to identify clinical variations and opportunities to reduce resource consumption and increase throughput in the organization. Physician-driven collaboration with the hospital is key to maintaining hospitals' profitability through clinical cost containment while minimizing the potential of compromising care. Using physician-directed process improvements, the hospital can make data-driven decisions that reduce the use of hospital resources, obviate costly errors and control variations in care delivery that compromise medical outcomes.
Assessment Components
In this process there are over 300 key checkpoints critical to understanding the level of preparedness for each of the seven assessment categories. Each of the 300 indicators can be reviewed, weighted and scored numerically to gauge readiness. In addition to the clinical performance data, the approach should include web-based surveys, data requests, workshops/interviews, capacity mapping and process reviews to identify both operational and strategic actions required to move forward with a coordinated care delivery model design.
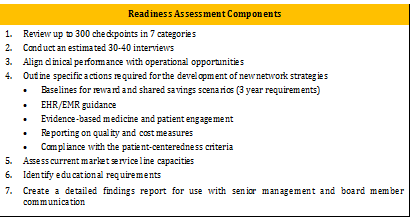
Readiness Assessment Components
1. Review up to 300 checkpoints in seven categories
2. Conduct an estimated 30-40 interviews
3. Align clinical performance with operational opportunities
4. Outline specific actions required for the development of new network strategies
- Baselines for reward and shared savings scenarios (3 year requirements)
- EHR/EMR guidance
- Evidence-based medicine and patient engagement
- Reporting on quality and cost measures
- Compliance with the patient-centeredness criteria
6. Identify educational requirements
7. Create a detailed findings report for use with senior management and board member communication
(Right click on image for a larger view)
Readiness Assessment Time frame (4-6 weeks)
The Readiness Assessment should be customized to incorporate any work already completed or in-process. Cost and quality data currently collected can be utilized and further analyzed in the assessment. This in combination with the newly obtained assessment results will complete the readiness picture. It is critical that this assessment be done in a concise time period. The following identifies time frames for activities to be completed within 4-6 weeks.Weeks 1-2
The initial weeks are a time to do a behind-the-scenes review of operations and data within the seven areas of readiness. The internal and external stakeholders should be identified for involvement in the assessment. A series of interviews can be conducted with key senior leadership and other professionals identified. The interviews focus on questions that align with the seven areas of accountable care priorities as well. These interviews will be designed to uncover a broad understanding of the hospital and physician general operations and integration. The interviews will also serve to enhance communication, build relationships and identify concerns. The strengths and weaknesses of clinical coordination and integration can be determined and the initial opportunities for enhancements identified. A technical assessment should be done of the quality and cost data. This assessment will identify variations in delivery of care and consumption of resources
Weeks 3-4
During these weeks, the data and information collected can be collated and analyzed. This includes scoring of all the check points within the seven areas. The scoring system can help identify the lower areas that need to be progressed to full readiness. Once the full picture is revealed, the leadership team can begin outlining actions required to maintain areas of high effectiveness and address areas of low readiness. This calls for discussion and dialogue to create innovative approaches to move forward.
Weeks 5-6
Presentations of identified findings and opportunities to validate them with can be made to stakeholders and generate additional ideas and input. There may also have been some educational needs related to accountable care identified for key groups or individuals that can be delivered in conjunction with the organizational results.
Moving toward 2013
Following the data collection and planning phases of the readiness assessment it is critical to establish ongoing monitoring, training, coaching and development of processes to capture the requirements for clinical integration/sharing strategies, primary care framework and performance/quality reporting.The leadership team and identified stakeholders can use the results to build scenarios and create new possibilities to achieve desired outcomes. The readiness assessment is the basis for the continued planning and action. As new information becomes available the leadership team must have the capacity to be flexible and adjust to new information and circumstances. Readiness assessment findings will assist healthcare leaders in making informed decisions and developing focused strategies as healthcare regulatory change begins in 2011. A comprehensive approach such as this one, is necessary if healthcare organizations want to not only “Survive but Thrive” through healthcare reform.
Learn more about Verras Consulting.

