Evaluating the Medicare demonstration programs
The Patient Protection and Affordable Care Act health reform legislation created several new types of provider arrangements that many hospitals and physician groups are evaluating. These organizational structures are intended to enhance the ability of hospitals, physicians and other types of providers to work together to enhance quality and reduce costs.Of these structures, accountable care organizations, or ACOs, have received the most notice. Conferences on ACOs are sold out; newsletters about ACOs are oversubscribed, and virtually every healthcare meeting has at least one speaker on ACOs. Consultants are begging hospitals to form ACOs before their competitors do, warning of precipitous losses in admissions to competing hospitals that have formed ACOs.
The other new provider arrangement is gaining significantly less attention. The bundled payment pilot program allows hospitals to work with physicians to reduce costs, and to pass along some of the cost savings back to the physicians. While far less grandiose that an ACO, participation in the bundled payment project may entail less risk and yield for better results for some hospitals. Since an organization cannot participate in both programs, it is important for hospitals to evaluate both alternatives before committing to either of them.
Accountable care organizations
In an ACO, the contacting entity is responsible for the health of the population, which is defined as patients who receive care from primary care physicians who are part of the ACO. All providers continue to be paid by Medicare through their normal payment methodology. The ACO will presumably implement care management processes that improve the health of the population while maintaining quality and reducing cost.
The payments made by Medicare for services provided to this population are compared to a target established by CMS that takes into account the severity of illness of the population. If the cost of the ACOs patients is more than 2 percent lower than the target, the ACO can receive a bonus payment of half of the cost savings, with Medicare retaining the remainder. Various laws and regulations concerning payments to providers and ability of providers to form organizations are expected to be reduced or waived to allow these organizations to be created.
In many ways, ACOs resemble Medicare Advantage plans. While patients don’t enroll in an ACO as they do in the MA plans, the overall health expenditure budget for the ACO is determined by CMS and is likely to be computed using the same severity adjustment methodology as used for MA plans. ACOs will also be required to implement quality measurement processes and reporting to satisfy CMS requirements. Because of these requirements, the infrastructure needed for an ACO will also be significant.
Bundled payment pilot
The bundled payment pilot program has a significantly different emphasis. While ACOs concentrate on the care of the population, the bundled payment program focuses on reducing costs of hospital services, and reducing hospital and physician utilization. It does this by reducing the current legal barriers to sharing cost savings with physicians, allowing them to participate in cost savings that they help to generate. These savings may come from reductions in hospital costs such as medical devices or prostheses, or through improvements in processes that reduce length of stay or the number of readmissions. While ACOs are focused primarily on primary care physicians and only peripherally involve specialists, the bundled payment project concentrates on the specialists who provide most of their care within the hospital. These cost savings accrue directly to the hospital, and can be shared with the physicians but need not be shared with Medicare.
A bundled payment contracting organization will be required to accept a discounted payment for all providers involved in services to the covered patients. This discount will be determined by the contracting organization as its bid to participate in the pilot. A “bundled” payment will be made by CMS directly to the contacting organization, which is responsible for dividing the payment among the physicians, hospitals, and other providers involved. The hospital, physicians and post-acute providers will not be paid separately by CMS for these services, and must receive payment from the contracting organization as a distribution from the bundled payment. Therefore, a significant infrastructure will be necessary for these organizations to adjudicate payments to these providers according to the methodology determined by the organization, and to provide for the quality reporting and other administrative services.
Comparing the alternatives
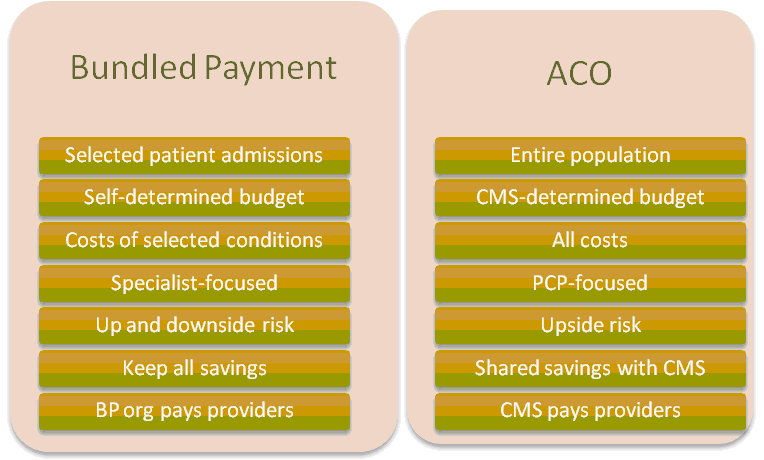
A chart summarizing the major differences between the two types of organizations is shown in Figure 1 below. Other differences are described below.FIGURE 1
Dollars in play
The amount of money involved in ACOs is significantly greater than that involved in a bundled payment project. In an ACO, the contacting organization is responsible for the entirety of the healthcare costs of its assigned population. Since Medicare annual expenditures per enrollee were $11,093 in 2009, the cost of a population of 5,000 Medicare members would approximate $55 million annually. Obviously, even the small reduction in these costs could create significant revenue for the contracting organization, and the lack of downside risk under the current demonstration parameters would limit the organization’s exposure to the significant risk associated with even a small increase in cost or utilization of this population.
The opportunity for financial reward in an ACO comes from incurring costs for the population that are lower than a risk adjusted benchmark for that same population computed by CMS. The benchmark in an ACO is not based on the actual cost of the ACOs patients, but rather a severity adjusted benchmark computed by CMS. While the severity adjusters do correlate with cost, a large proportion of cost variation is not explained by severity adjusters. Even a small difference between this benchmark and the ACO’s actual experience would be highly significant in terms of total dollars. This leads to two conclusions: first, that randomness plays a large part in the financial success or failure of these organizations; and second, that these organizations should make all possible attempts to estimate the CMS benchmark, and compared to their actual patient costs, before embarking on forming an ACO. This is the only way that reasonable estimates can be made of the financial results of the ACO. This is a complex task, but the stakes are high. Data analytics and actuarial science should play a key role here.
In addition, it is expected to take several years for CMS to obtain and analyze the results of an ACO, and to make any applicable cost sharing payments to the ACO. This means that the ACO must be sufficiently well capitalized to incur its startup and operating costs for a number of years before potential of receiving any additional revenue.
For the bundled payment pilot, the financial risks and rewards are considerably more modest. The savings that the organization can realize comes solely from its ability to reduce hospital costs, and also from reductions in payments (through changes in payment rates or utilization levels) to all providers who provide services to the demonstration project’s patients. From previous similar demonstration projects, the savings have arisen from the consolidation of medical device and prosthesis purchases, reduction in hospital lengths of stay, decreases in utilization of consulting physicians, and other similar actions. Some hospitals have achieved multimillion dollar savings for these initiatives, and have shared those savings with the physicians who helped create them. Others hospitals have achieved little or no savings, while having to bear the administrative costs of the organization.
In evaluating this characteristic of the programs, it’s obvious that ACOs will offer a greater possibility of financial return if their initiatives are effective. On the other hand, ACOs are subject to significantly more randomness because of the CMS severity scoring adjustment, and are therefore subjecting themselves to a higher degree of risk. By contrast, the rewards of the bundled payment program are significantly more modest but are almost entirely within the control of the contacting organization. Therefore, ACOs may appeal to an organization having a lower aversion to risk, while the bundled payment option may be more appealing to more risk-averse organizations.
Patient population
The patient populations involved in each of these programs are significantly different. In an ACO, the organization is responsible for the health of the population, including significant expenses incurred outside of a hospital. Population health management is generally not within the “sweet spot” of hospital competencies since hospitals are more focused on treating patients whose conditions have required hospital services, rather than finding ways to help members of the population avoid the need for those services. Only about 44 percent of Medicare expenses are incurred in a hospital setting, which makes it difficult for the hospital to have a significant effect on them. Instead, the hospital must work through the physician network, relying primarily on primary care physicians, to provide the majority of care to the community. However, many primary care physicians are only loosely affiliated with the hospital, and provide most of their services and receive most of their income from their office practices. This may make it difficult for a hospital to create changes in the health status of patients who do not come to the hospital.
In addition, patients with chronic diseases (diabetes, congestive heart failure, COPD, hypertension, etc.) account for more than 50 percent of healthcare costs (and often much more, depending on how they’re categorized). Significant savings can be realized a properly caring for these patients, and by providing a care infrastructure to monitor their medical conditions and take corrective action when appropriate. Most of this preventive care occurs outside of a hospital; indeed, a major objective of that care is intended to prevent the need for hospital services. Many hospitals do not have the knowledge or infrastructure to provide the services, and will have to depend on others to design, coordinate, and implement these care management programs. There will inevitably be a startup period during which various programs will be tried, evaluated, abandoned, and replaced. During this period the ACO will incur its organizational costs, but is unlikely to create any meaningful cost savings.
Under the bundled payment project, the patient population is limited to those patients receiving hospital services. Hospitals know how to care for these patients, so achieving success requires making relatively minor changes in the way that services are delivered, rather than requiring the complete paradigm shift.
Alignment of financial incentives
The financial incentives of the ACO run directly counter to those of the hospital, since the financial objects of the ACO are to reduce the use of hospital services, while the financial objectives of the hospital are to increase the use of those services. This dichotomy led to the failure of many managed care organizations in the 1990s, and would require significant change in mindset of most hospital financial managers, boards of directors, shareholders, bond rating agencies and others with a financial interest in the hospital. Although these conflicting incentives may be resolvable, their existence creates an initial barrier to effective care of the most costly patients.
By contrast, the financial incentives of the bundled payment project are directly in line with those of the hospital. Every hospital wants to find ways to reduce costs and lengths of stay of Medicare patients. The bundled payment project enhances this ability by allowing the hospital to share the savings with physicians, thereby creating an incentive for physicians to work with the hospital to achieve these savings. Therefore, this project does not require a change in hospitals incentives; rather, it reinforces the existing incentives.
Physician relationships required
The basis for forming an ACO is the assignment of patients from PCPs who are part of the ACO. Unless they are employed by the hospital, however, most PCPs do not have close working relationships with hospitals, since most of their practices are office-based. Attracting these physicians into a hospital based organization, especially one whose financial results are as unpredictable as an ACO, may be a challenging task. In addition, PCPs may be concerned about the effect that participation in an ACO may have on the perception of the PCPs' patients. While some Medicare patients may be attracted to a PCP who participates in an ACO that is focused on improving overall patient wellness, other patients may view the ACOs an organization attempting to save money by limiting the services provided to its patient population. The latter group of patients may not wish to utilize a primary care physician who participates in an ACO. Therefore, establishing relationships with the PCPs who are essential to the creation of the ACO may be challenging.
Hospitals in the bundled payment project will be dealing primarily with medical specialists who provide services within the hospital, rather than with PCPs. Relationships with these physicians may already be well established, and the financial effects of participation are relatively easy to predict and explain. The current and previous Medicare bundled payment demonstration projects have achieved documented results, many of which have been advantageous to the physicians participating in them. One negative consideration for physicians is that they will no longer be paid directly by Medicare at the physician fee schedule rates; instead they will be paid by the contacting organization at rates negotiated with that organization. The details of these rates and payment process are obviously of concern to the physicians, and should be worked out in advance of expecting any physicians to agree to participate.
Infrastructure and organization costs
The infrastructure and organization costs of both types of organizations will be considerable. An ACO will require an entire public health infrastructure that is able to provide generalized services to an entire patient population. Critical to the success of this effort will be the establishment of patient management programs for chronic care patients, which represent more than 50 percent of healthcare costs, and without which no ACO can hope to achieve meaningful cost savings. The extent of these programs, and that the resources required to manage the operations and finance of the organization and satisfy the required reporting requirements of CMS, are difficult to estimate but will be significant. One function that an ACO will not have to assume is payment of the providers, since providers participating in an ACO will continue to be paid by CMS at the existing Medicare fee schedule amounts.
In the bundled payment project, the contracting organization receives the bundled payment from CMS and is responsible for distributing that payment among all providers who provide services to covered patients. This will require the establishment of an entire provider payment system that can receive claims from these providers, adjudicate them based on the relevant contracts, and make the appropriate payments to the providers. In addition, the organization must build the infrastructure necessary to manage the cost reduction projects, bringing together hospital and physician personnel with the expertise to achieve these savings. While this infrastructure is expected be less extensive than that required to establish an ACO, it is certainly not insignificant nor inexpensive.
Effect on patient volume
Maintaining patient volume and market share is always a critical objective for a hospital. However, “market share” becomes more difficult to define in an ACO setting in which the objective is to reduce the volume of hospital services provided. If an ACO is successful, hospital revenue will decrease. Presumably of some of this decrease will be mitigated by receipt of CMS bonus payments reflecting the reduction in population costs below the target amounts. Arguably, ACOs that align themselves with a large number of primary care physicians may increase their volume by drawing from a larger patient base; however this will only occur if the ACO involves PCPs whose patients would otherwise have received services from a different hospital. In addition, as mentioned previously the effects on a PCP practice of participating in an ACO are unclear. Some patients may view the arrangement positively, and may wish to utilize a PCP who participates in an ACO. Others may view it negatively, and may leave such a PCP practice. Thus, the effect of participating in an ACO on an organization’s patient volume is difficult to define or predict.
The effect of participating in a bundled payment program is easier to define, but no less difficult to predict. Since patient volume is still measured by the number of patients utilizing hospital services, an increase in patient admissions for bundled payment services is still financially beneficial to the hospital. While previous bundled payment demonstration projects have not created increases in patient volume, rebates paid by CMS to Medicare beneficiaries who utilize bundled payment providers may create increases in volume for those providers.
Summary and conclusions
An ACO is a significantly larger undertaking than participating in a bundled payment pilot program. While its downside risk is limited by the current parameters of the Medicare law, its administrative costs and effects on hospital utilization can be considerable. In addition, it is population focused, not patient focused. Therefore, ACOs may end up being formed by large hospital systems that dominate the local markets, have strong existing affiliations (or ownership) with primary care physicians, and may already have significant public health programs in place. These organizations could withstand the initial financial losses that are likely to occur during its initial operations, and potentially on an ongoing basis. Smaller hospitals will unlikely to have the financial strength to capitalize such an organization, nor the PCP and public health infrastructure to make them successful.A bundled payment pilot, however, may be applicable to be significantly wider group of hospitals. While the infrastructure costs will be considerable, participation does not involve the paradigm shifts necessary in financial management and delivery of care that are required of an ACO. A bundled payment pilot may allow a hospital to increase its alignment with physicians participating in the pilot, since allows them to be directly financially rewarded for their efforts in reducing hospital costs. Hospitals having good relationships with their medical staff members may find bundled payment programs an advantageous way reduce costs and increase physician alignment.
Singletrack Analytics is a healthcare financial and data consulting firm specializing in assisting healthcare providers and purchasers to achieve success through better use of data and analytic techniques. We have worked with hospitals, integrated delivery systems, payers and others to design payment systems, data warehouses, reporting solutions, and financial analyses. We understand the healthcare financial environment and the tools and techniques required to achieve success. For information about Singletrack Analytics, please visit our website at www.singletrackanalytics.com or email at info@singletrackanalytics.com.

