The following content is sponsored by Health System Advisors.
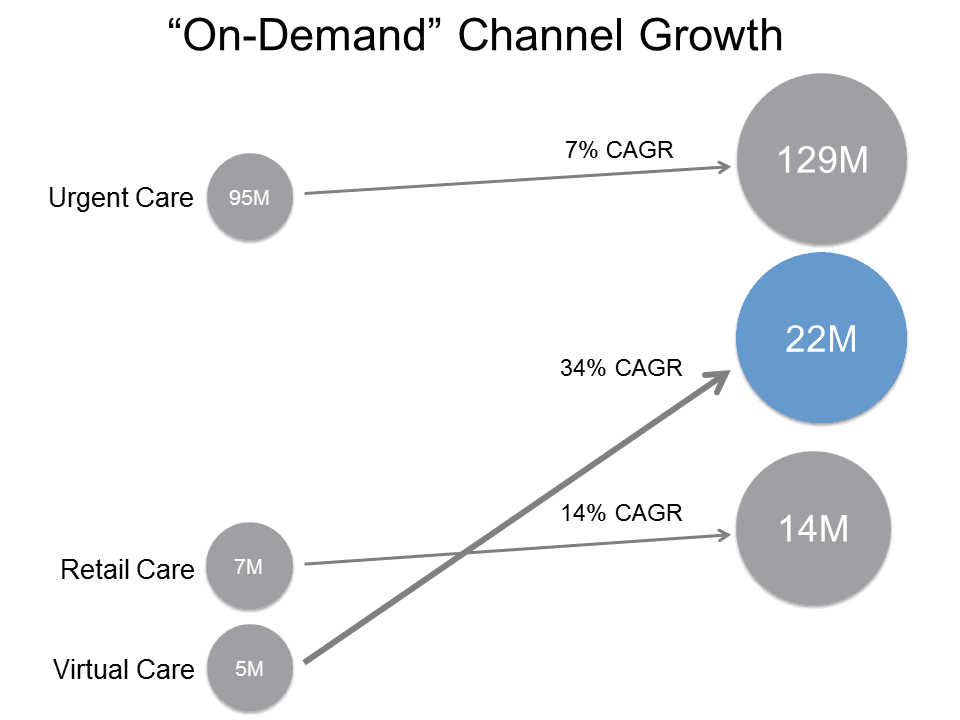
A growing market segment is demanding unscheduled access to primary healthcare services without consideration of health system or pre-existing clinician relationship. This population segment has given rise to a new set of "on demand" primary healthcare delivery channels. These on demand delivery channels have strong growth projections (ranging from 6.5 to 34 percent annually) over the next several years creating an opportunity or threat for the traditional primary care providers and the health systems.
There are numerous reasons for the growth of on demand delivery channels. Chief among these reasons are the rising importance of convenience, access outside the 8:00 am to 4:30 pm typical work hours and the empowerment of the consumer in directing their own health. Consider for instance, people under 40 years old are almost 50 percent more likely to not have an established primary care physician relationship and instead access primary healthcare through urgent care, retail and virtual providers. Health systems that want to remain relevant and care for this growing population segment must understand this group's demands and embrace innovations in primary healthcare delivery.
To date, health systems have been slow to respond. While health systems have gone on a primary care employment binge, they only operate 28 percent of the urgent care centers,1 are only recently actively partnering with the major retail operators,2 and have almost no presence in virtual primary healthcare delivery. This void in serving the on demand care is rapidly being filled by technology companies, health insurers, venture capital and other non-traditional healthcare providers. Given the rapid growth rates and importance of the demographic, health systems must understand how they will participate in each of these on-demand delivery models.
While each on-demand delivery model is important for health systems, this article focuses on the lessons learned in the asynchronous virtual primary healthcare delivery model including experiences from Zipnosis, a leading virtual primary healthcare delivery provider.
Virtual primary healthcare
Virtual primary healthcare is the use of electronic mediums to deliver primary care including: education, prevention, diagnosis, treatment and disease management
There are two major models of virtual care:
• Synchronous: models that connect people and providers in real-time
• Asynchronous: models that deliver care to people without requiring real-time interaction
Synchronous care uses technology like phone, video or chat to connect patients and providers (and sometimes clinician-to-clinician) in real-time for a wide-range of medical conditions. Synchronous virtual care, while a novel application of technology, improves clinical efficiency only to the extent it reduces travel for the clinician or patient. In rural areas with large distances, traditional synchronous telemedicine adoption is widespread; however in the urban areas where most of the population lives, there is less efficiency to be gained and the increased transaction costs have outweighed the benefits.
Asynchronous care solutions create efficiency in an entirely different way. Asynchronous care focuses the clinician's interaction to the most essential elements, allowing batching of the clinician's time to capture scale economies. Starting in the form of secure e-mail, asynchronous primary care models made a major jump in the 2000's as technology took the unstructured e-mail and incorporated evidenced-based protocols and linked the patient's medical history in a highly structured manner. This transition allowed asynchronous virtual care to use sophisticated computer algorithms (and in some cases consumer devices) to collect all the necessary information and organize it efficiently without direct patient-clinician interaction. Today, clinicians still review the information and make a diagnosis and treatment, but their role is limited to clinician decision-making, not documentation or administrative tasks.
The shift from synchronous to asynchronous has major advantages for virtual primary healthcare. For the patient, asynchronous models provide high quality, efficient and convenient access to primary care anytime and anywhere they have an internet connection. For the clinician, diagnosis and treatment time can be compressed by a factor of 10 or more.
Lessons learned in virtual primary healthcare
Zipnosis is a leader in the virtual primary healthcare delivery revolution. Founded in 2009, Zipnosis charges $25 to patients to diagnose and treat common primary healthcare conditions without a face-to-face encounter. In place of a typical scheduled physician office visit or trip to urgent care, Zipnosis uses an adaptive, automated online interview to collect the patient's medical history and summarize the data for clinicians who then review the evidenced-based diagnosis and treatment recommendations and make final clinical decisions.
After five years leading the revolution, Zipnosis offers six insights about this primary care delivery channel and why health systems should be interested in integrating some form of virtual care in their delivery platform.
Learning 1: Unique population segments
Zipnosis users are a rapidly growing population segment seeking to address their primary healthcare needs in very different ways than the traditional healthcare industry has allowed. For most of the patients that use virtual primary healthcare, convenience and time-savings dictated the decisions. This is a population that does not use the traditional scheduled primary care office model for their care. In fact, more than 60 percent do not have a primary care physician. Moreover only 30 percent of the patients would have sought care in a primary care clinic had a virtual care option not been available.3 This mentality is not just a phenomenon of the millennials; the typical Zipnosis user is a 37 year old female who is the healthcare decision-maker for her family. Zipnosis experience shows the virtual primary healthcare users are not just the tech-savvy, but those that are used to virtually accessing services from other industries like banking, travel and retail.
Additionally, the patients attracted by a virtual primary healthcare delivery model are often new patients for the Zipnosis' system partners. More than half of all Zipnosis patients referred for further diagnosis or treatment to a partner system are new to that system.4 This new patient percentage is an important consideration for health systems that want to grow into new markets or population segments. With a virtual access point, the health system can provide 24x7 access to populations both in and outside its traditional markets.
Learning 2: Direct downstream health system value
Virtual primary healthcare does not treat all primary healthcare conditions. About two-thirds of all patients that seek care through Zipnosis must be referred to another form of care, typically an ER, urgent care or primary care office. While this percentage is declining as the number of conditions treated by Zipnosis expands, there will continue to be downstream referrals from Zipnosis. Referrals from simple laboratory diagnostics to complex imaging diagnostics to acute events means the traditional components of Zipnosis health system partners benefit from the growth of Zipnosis. Depending on the relationship with the health system, these referrals can be very sticky with the ability to schedule appointments and transition the demographic and patient history directly through Zipnosis. Unlike the other primary healthcare delivery channels, virtual has the unique potential to provide immediate access to its health system partner's scheduling system for referrals, follow-up, diagnostics or other services. Measuring the immediate downstream economic value (in the form of contribution margin) of a typical virtual primary healthcare patient ranged from $14 to $26 depending on the setting.5,6
Learning 3: Increased clinician productivity
Asynchronous virtual primary healthcare delivery models are highly clinician efficient. Zipnosis' experience has demonstrated 10-20 times increase in clinical capacity for primary healthcare visits. This 10- to 20-fold efficiency gain is created by using an adaptive interview to create a full history, description of the symptoms, document 90 percent of the medical record, and using complex evidenced-based algorithms, recommend best practice treatment choices to the clinician. For each visit, the clinician is presented with a series of easy-to-select choices, based on the latest evidenced-based treatment guidelines. Because the clinicians are used only for making clinical choices, not administrative tasks like documentation or calling in a prescription, a clinician requires only an average of 2.5 minutes per patient encounter.
In addition to this dramatic efficiency increase, the asynchronous nature means these 2.5 minute clinician time blocks can be fit into any existing open time that clinicians have during the day.
Unlike synchronous visit models that demand dedicated staffing and high start-up costs, Zipnosis has demonstrated asynchronous virtual primary healthcare start-up and scaling costs are minimal. One of their health system partners was able to diagnose and treat over 8,000 patients without hiring a single FTE. Instead, they used marginal clinical capacity in existing employed primary care clinics and urgent care. Moreover, a virtual primary healthcare model can be integrated into a health system's market in less than 90 days. Contrast this with a health system's option of a two-year, $2 million+ development plan for extending an EMR7 or building a similar solution from scratch without a proven record demonstrates how far ahead the leaders in virtual care are today.
Learning 4: Improved quality and satisfaction
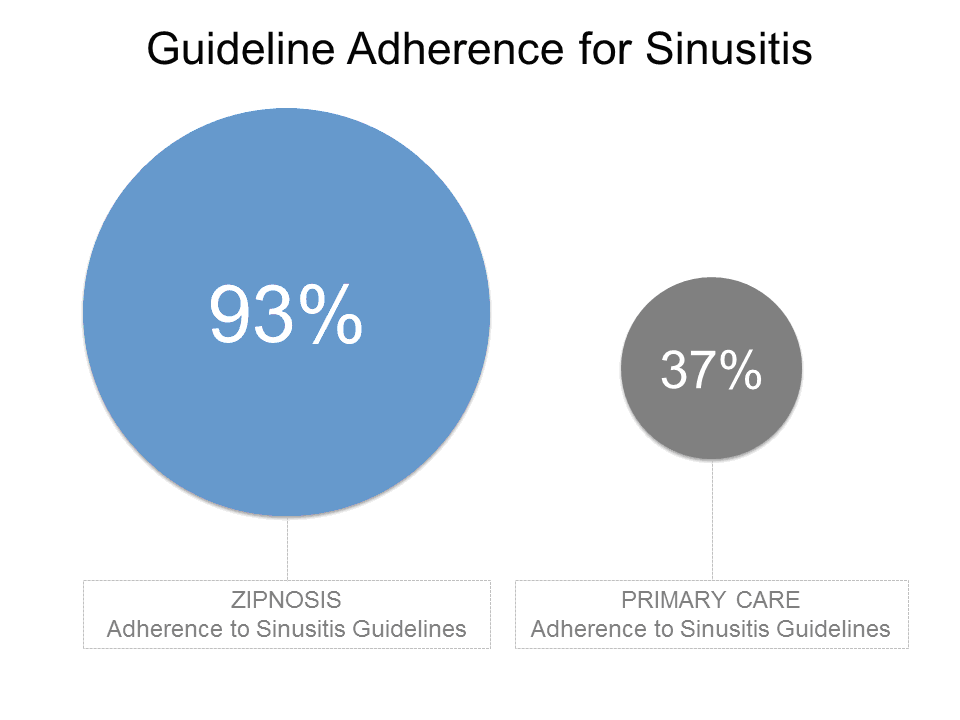
Algorithms used in Zipnosis' di agnostic and treatment process are based only on nationally accepted, evidenced-based protocols. While each diagnosis and treatment plan is individually reviewed and received sign-off by a clinician, the software system is designed to restrict clinician choices to only those that are clinically appropriate per guidelines and the latest evidence. Moving off protocol must then become a conscious choice rather than an unconscious error. As a result, the Zipnosis adherence to clinical guidelines is 93 percent for the most common conditions which are two times the adherence of a typical primary care practice setting.8 Moreover, adherence reporting is integrated into every treatment, making it possible to take immediate corrective action rather than wait for a manual chart review that may occur only annually. In an environment of population health and increased quality transparency, encouraging patients to use models that adhere more closely to evidenced-based diagnostic and treatment plans is valuable.
Additionally, patient satisfaction is far higher than other models. Virtual primary healthcare is experiencing tremendous growth because it fundamentally meets a need in the market for quick, easy and immediately convenient access to primary care. For Zipnosis this has translated into a 95 percent satisfaction rating. More tellingly, 91 percent of patients surveyed recommended Zipnosis to three or more friends. In the age of social media, this level of word-of-mouth advertising is unbeatable.
Learning 5: Increased scope of care
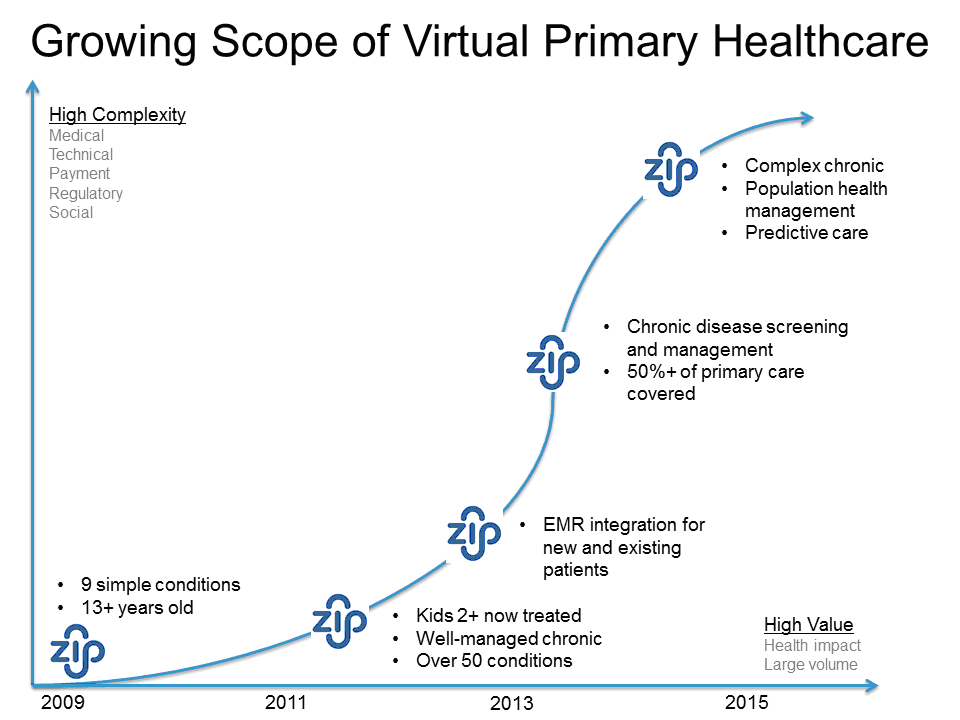
One of the biggest hurdles for asynchronous virtual primary healthcare models has been the scope of care covered. The initial scope of care included the most common health problems like sinus and bladder infections, but these still only represented a small fraction of the total primary healthcare delivered through other channels. However, as more and more objective clinical data flows through mobile phones, remote sensors and wearable computing, Zipnosis and other computer-assisted service models are integrating that data into their digital backbone and increasing the care capabilities.
Zipnosis scope of care has steadily grown. From 2010-2012, Zipnosis treated nine simple conditions for patients over 13 years old. In 2013 it added 40 more conditions— including the ability to upload an image for dermatology conditions — and treatment for kids as young as two years old. In 2014, Zipnosis will launch another 20 acute conditions, and more tellingly, a fully virtual screening and management service for its first major chronic disease. Unlike other primary healthcare delivery channels that must make massive capital and human/process investments to change or add new modes of care, Zipnosis' technology-driven approach allows it to rapidly add new service lines.
Learning 6: Positioned for the future and experiencing rapid growth
Virtual primary healthcare delivery model is projected to grow nearly 35 percent per year over the next several years.9 The market leaders are seeing many times this growth. For instance, Zipnosis has seen three times the growth in volume in its major markets the past three years as more as more consumers become aware of the service. Moreover, under a population health reimbursement environment, virtual primary healthcare is poised to grow even faster as the model is proven to reduce the cost of care. Both the direct cost and the total cost of care, including follow-up care is significantly lower than the alternative primary healthcare delivery channels. For the typical Zipnosis patient the total cost of care is reduced by nearly $100.
As a result, virtual care models can be used to effectively triage populations for which health systems have taken healthcare financial risk. Using different co-pay levels or other incentives to move patients to a virtual care model can keep a portion of the population out of more expensive treatment environments.
Health systems must be involved to remain relevant
A growing segment of the population is turning to non-tradition models of healthcare. In primary healthcare this is most apparent in the growth of the unscheduled/on-demand care models. Virtual primary healthcare represents the fastest growing of these, and one in which health systems must quickly figure out how to participate. Those systems that do embrace these alternative channels stand to gain new populations and build capabilities to increase their market relevance. Those that ignore the channel are destined to spend more and more resources trying compete directly for a declining market of traditional primary care delivery channels. Fortunately for the health systems, the current virtual primary healthcare market leaders appear to be content to stay technology and service companies, leaving an opening for traditional health systems to partner in the virtual care delivery models. But health systems must act fast.
1 Urgent Care Association of America.
2 Stempniak, M. “Retail Clinics: Threat or opportunity?” Hospitals and Health Networks. October 1, 2013.
3 65% of the patients say they would have used an ER, urgent care center, walk-in clinic, or retail center if a virtual care model had not be available.
4 In a 2013 study conducted by one of Zipnosis’ health system partners, 55 percent of all patients referred through Zipnosis were new to the system with no prior contact with the health system’s facilities or directly associated physicians.
5 K. Lovrien, L. Peterson, et al; The Case for Virtual Care; Health System Advisors, June 2013.
6 This means that for every patient that starts a visit with a virtual provider there is an estimated $14-$26 of new contribution margin for traditional health system and physicians generated from the average number of direct referrals and typical payer mix.
7 Connecting with Patients Online: E-Visits, Gidwani et al, December 2012
8 Zipnosis adherence to protocol compared to primary care physician offices treatment of adults with acute bronchitis (2013); American Journal of Medical Quality
9 Heidenreich, et al; Health System Strategy: Remaining Relevant by Building Primary Care Delivery Beyond Physician Employment; Becker’s Hospital Review, March 2013