A high level overview of quality metric market trends and value drivers from a valuation firm’s perspective.
In a value-based reimbursement environment, critical success factors have shifted from financial performance toward cost efficiency and quality performance benchmarked to national standards. With the growing influence of quality outcomes measurement organizations, such as The Joint Commission, LeapFrog, and U.S. News & World Report, hospitals and healthcare providers are increasingly using quality and cost to distinguish themselves and the value they add to the market. This means the utilization of quality metrics to gauge performance is more important than ever.
With this level of emphasis, the selection of the metrics to be measured, the determination of the associated benchmarks and stretch goals, and analysis of historical performance cannot be overlooked. In fact, from a valuation firm’s perspective, the quality metrics and their associated attributes are the main value drivers in determining the maximum fair market value (“FMV”) compensation payable to physicians for quality outcomes and in creating a meaningful quality improvement program that is consistent with the market.
Further, based on analysis of quality payments to physicians in the market, as well as, analysis of hospital pay-for-performance programs funded by both governmental and commercial payors, certain program attributes related to the metrics have been consistently observed when incentive dollars are rewarded for quality.
So, how do your quality improvement program’s metrics stack up? Take the quality metrics quiz to find out.
What to know about quality metrics: The quality metrics quiz
QUALITY METRICS QUIZ
How Do Your Quality Improvement Program’s Metrics Stack Up?
1 Did management select the metrics based on the needs of the service line, patient population or facility?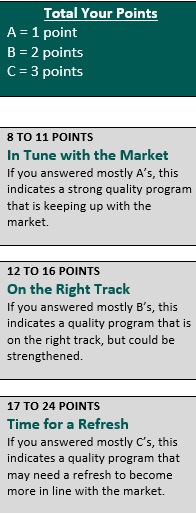
A. Yes
B. Some
C. None
2 Is there a substantial number of meaningful metrics?
A. Yes
B. Some
C. None
3 Are the participating physicians considered independent contractors or, if employed, is their professional compensation at-risk (i.e. $/work relative value unit model, no fixed/guaranteed salary)?
A. Yes
B. Some
C. None
4 Are the physicians (versus the hospital’s staff’s) primarily responsible for impacting the selected metrics?
A. Yes
B. Some
C. None
5 Are the metrics outcomes-based (i.e. clinical outcomes, patient satisfaction, and/or efficiency metrics) versus process metrics (i.e. adherence/compliance to protocols, etc.)?
A. Yes
B. Some
C. None
6 Are the metrics nationally measured/supported by credible medical evidence (compared to metrics that were established internally or created to meet a hospital-specific objective)?
A. Yes
B. Some
C. None
7 Do the metrics require measurable superior performance (i.e. national/industry top decile performance)?
A. Yes
B. Some
C. None
8 Are the metrics maintenance goals (i.e. metrics in which historical performance meets or exceeds national top decile or internal superior performance) compared to hard to achieve goals?
A. None
B. Some
C. Yes
This article is not intended to be, nor should it be used as, a substitute for legal, valuation, or regulatory advice.
Nicole Montanaro is a Manager in the Professional Services Agreements division at VMG Health, LLC in Dallas, Texas and has performed hundreds of quality incentive compensation valuations. Her area of expertise is dedicated to performing valuations of compensation agreements within the healthcare industry (nicolem@vmghealth.com)