"Systemness" describes effective alignment among core characteristics of a health care provider's organization design: structure, culture, capabilities, processes, people and rewards.
The goal: to produce measurable value in the patient experience, per capita cost of care, and population health. Systemness is an ideal state for the industry, but the path for achieving it isn't always clear.
Relatively few large health care provider organizations have achieved optimal systemness. Instead, most are siloed; they continue to make decisions and conduct their operations at the facility, department, geography or service line level rather than the system level. But health care reform and provider consolidation and integration have created significant pressure for greater efficiencies and improved outcomes -- goals that a systemness approach can help achieve.
Human resources executives play a major role in helping health care providers achieve systemness. Employees are both the organization's single greatest cost and its greatest differentiator. Therefore, HR executives who can identify symptoms of workforce fragmentation and target coordinated solutions to gain the best possible ROI from employees can create significant efficiencies that are the hallmark of systemness.
Our experience helping HR leaders pursue the benefits of systemness suggests there are five key areas in which they may add the greatest value, ranging from foundational to transformational.
1. Implementing a common job architecture
2. Effectively supporting mergers and acquisitions
3. Aligning physicians
4. Building new leadership capabilities
5. Embracing pay for performance
Implementing a Common Job Architecture
Job architecture is a mechanism for organizing jobs that includes components such as job families, functions, titles and codes. To achieve the financial and operational efficiencies required of health system integration, providers must manage their workforce for productivity and performance. Because you can't efficiently manage your workforce if you don't fully understand the roles and the incumbents, the organization needs some foundational practices in place.
This foundation can enable the more advanced human capital management practices required of systemness, including workforce analytics, career development, total rewards design and segmentation, staffing models and span of control analyses. Organizations then also have the ability to segment and measure, which can support performance management and incentive programs. Furthermore, a well-designed job architecture can easily expand to reflect the new responsibilities resulting from massive industry changes.
In fact, Towers Watson research shows that organizations with highly evolved talent management and reward practices are 1.5 times more likely to report financial performance significantly above their peers. These successful organizations have the necessary foundational practices that help create a highly evolved approach to talent management and rewards, including an organizationally consistent job architecture.
Effectively Supporting Mergers and Acquisitions
HR plays a critical role in supporting effective due diligence before a merger or acquisition. Post close, it helps plan, integrate and implement critical changes, including:
1. Evaluating the strategic deal rationale and fitness of potential candidate organizations — including their workforce and culture, leadership styles, talent management programs, cultural and communication styles, and HR and related workplace programs and practices that could affect integration. Employee survey results from candidates and acquirers can facilitate analysis of culture fit and leadership alignment.
2. Assessing potential costs — including the total cost of the target's compensation, pension, health care, retiree medical, and related workforce and reward programs.
3. Identifying and preparing staff to address the full range of integration issues — from identifying leaders and retaining key talent, to harmonizing workplace programs and managing the communication and change management strategy so critical to the success of any organizational change. Towers Watson research and experience with organizations in transition, including merger activity, shows that employees in such environments are especially critical both of communication from leaders and a perceived lack of career opportunity.
A key ingredient in this role is an M&A playbook that provides guidance to the HR team for the entire M&A process, including handling due diligence, assessing and integrating the people aspects of the transaction and documenting connection points with other corporate teams along the way.
Health care systems that still operate in a siloed manner can apply some of these same M&A processes to support their move toward systemness. Effective communication and change management strategies are particularly critical and can help articulate the sustainable value of the transformation.
Aligning Physicians
Physicians play a pivotal role in the organization. Are they doing the right things, are they being paid the right way, and is the organization getting the results it wants? HR can help the organization optimize the value of physician relationships through targeted investments in roles, rewards and results. HR can also play a key role in maximizing collaboration among physicians, non-physician leaders, and operational executives to assure fully aligned buy-in to the transformations that are needed:
1. Align structure and design of jobs and roles with strategic priorities. This includes development of strategies and approaches to align physician interests with organizational goals and "top of credentials" analysis and definition of roles among physicians, advanced practice clinicians (APCs), and other care delivery team members.
2. Provide compensation and benefits assessment, valuation and design. This includes the development of a physician rewards philosophy, governance and oversight; analysis and design of compensation programs for both employed and contracted physicians, including co-management, on-call, and administrative services arrangements; competitive market data analysis and benchmarking compensation structures and performance levels to market; analysis of outcomes of current compensation approaches to identify gaps between desired performance and actual outcomes, and ensuring regulatory compliance and fair market value compensation arrangements.
3. Identify and focus on key drivers of attraction, retention, engagement and performance. The factors that drive physician engagement are unique from those affecting other populations and include a particular focus on personal empowerment and career development. Because these drivers can vary widely from one system to the next, HR needs to provide an empirical fact base that will enable the organization to determine the potential ROI of various total rewards design alternatives for engaging and retaining talent. This analysis will help inform decisions about the most effective utilization of base salary, performance-based compensation, benefits, work-life balance and career development.
HR historically has ceded substantial decision-making regarding employed physicians to medical group management, but this has sometimes led to suboptimal value to the organization. To drive toward systemness, HR should bring the same management rigor to this critical workforce segment.
Building New Leadership Capabilities
There's no question that effective leaders are critical to systemness. In Towers Watson research and experience, leadership has been shown to be a top driver of employee engagement (both globally and in health care systems), and is linked with better outcomes – for patients and the bottom line. In addition, health care system employees who judge their organization as effectively managing cost, quality, and efficiency say that credible leadership plays a key role.
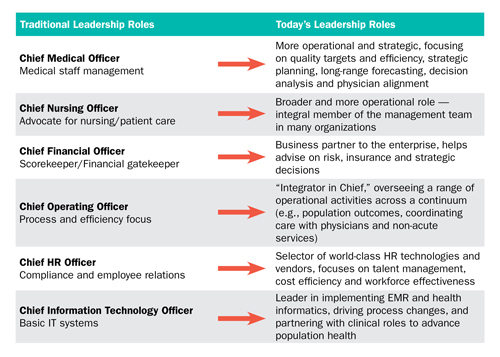
The requirements of effective leadership must change to meet the imperatives of an industry in transformation. Towers Watson experience shows a shift in competency requirements of leaders as well as a redefinition of traditional leadership roles in health care. Several prominent examples are highlighted below.
Many health care leaders are not living up to these new imperatives, and analysis of Towers Watson's normative database of employee opinions shows that many employees do not see their leaders as effective. In fact, employee opinions of health care provider leaders are significantly less favorable today than even two years ago, and key leadership attributes such as "understands business direction" and "concern for employee well-being" are among key areas in decline. Further complicating the challenge, many HR executives do not see their development programs as effective.
To change course, HR must do four things:
1. Segment leader roles to create the right development focus
2. Redefine and articulate the new expectations of leaders in the organization including the importance of effective communication and change management to align the workforce with the goals of the entire system
3. Assess and develop leaders against the new role requirements using the tactics that work best
4. Build a pipeline of leaders with the skills required for today's needs and critical for tomorrow's vacancies
Embracing Pay for Performance
The rapid movement toward revolutionary revenue models (ACOs, bundled payments, reference pricing, VBP, increased consumerism, etc.) threatens to squeeze or destroy traditionally lean operating margins. It is time for health systems to get serious about shifting a larger portion of employee total rewards costs from fixed (base pay, uniform merit increases, step-rates, etc.) to variable to better support sustainable margins. Not only will this better align costs with revenue, it also presents a potent opportunity to support the organization's evolution away from traditional cost-plus and fee-for-service operating models toward a culture of accountability for value. Performance-based rewards – aligned for executives, staff and physicians – are one of the most effective ways to achieve these goals.
In fact, Towers Watson research with health system employees who judge their organization as effectively managing cost, quality, and efficiency points to pay-for-performance as a top strength. Keys to success include clearly articulating the system's definition of value, defining critical performance drivers and metrics, holistically aligning performance-based rewards for key employee segments with those metrics and supporting their ongoing operation with effective change management and communication.
HR leaders have their work cut out for them to help their organizations achieve the promise of systemness. Those who accomplish this significant challenge will reap the rewards of market leadership in this next exciting chapter in the transformation of health care.
Donald Gallo is a Consulting Director in Towers Watson's Executive Compensation and Talent Management & Organizational Alignment practices. He can be reached at donald.gallo@towerswatson.com
Patrick Kulesa is a Global Director in Towers Watson's Research and Innovation Center. He can be reached at patrick.kulesa@towerswatson.com.
The views, opinions and positions expressed within these guest posts are those of the author alone and do not represent those of Becker's Hospital Review/Becker's Healthcare. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them.