If clinicians and care managers knew patients had difficulty with transportation access before he or she was admitted, it would go a long way towards improving patient outcomes, according to a new survey from Connance, Inc.
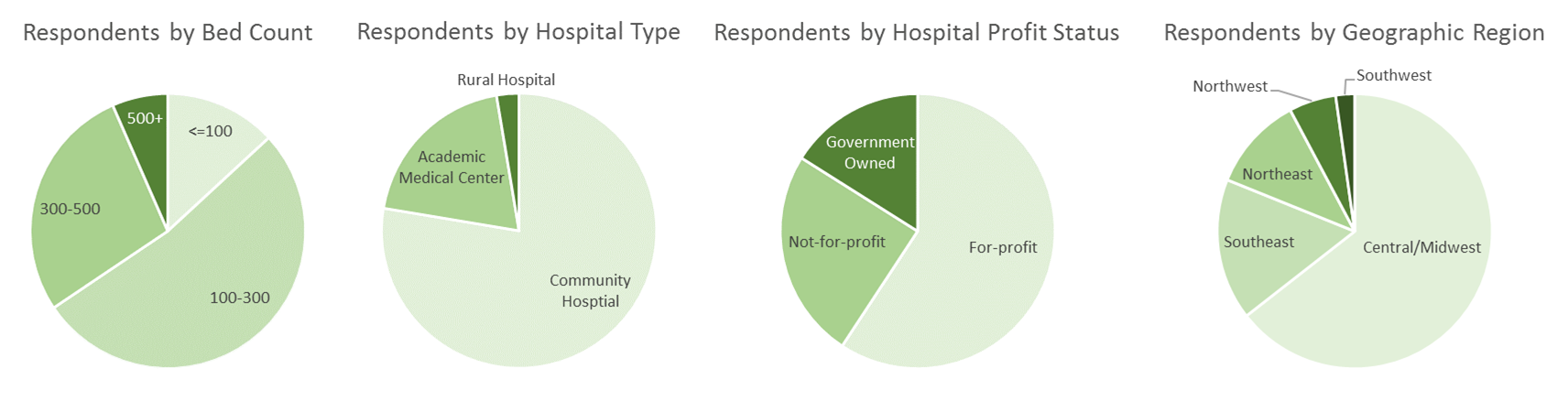
That’s just one of the findings from the predictive analytics company’s recent study. They asked 175 case managers, social workers, and clinical executives across the United States about the current availability and use of social determinants of health data. The survey findings suggest that knowing about transportation access, as well as other socio-demographic factors such as financial instability and food access, and knowing about it at the right time in the care process, can go a long way towards improving patient outcomes.
The right social determinant data...
In spite of significant investment in EMRs and population health systems, over 84 percent of case managers cite a meaningful gap in their access to appropriate SDOH information. While the vast majority of them have access to some social determinant information, such as aggregated data by zip code, it fails to meet their needs.
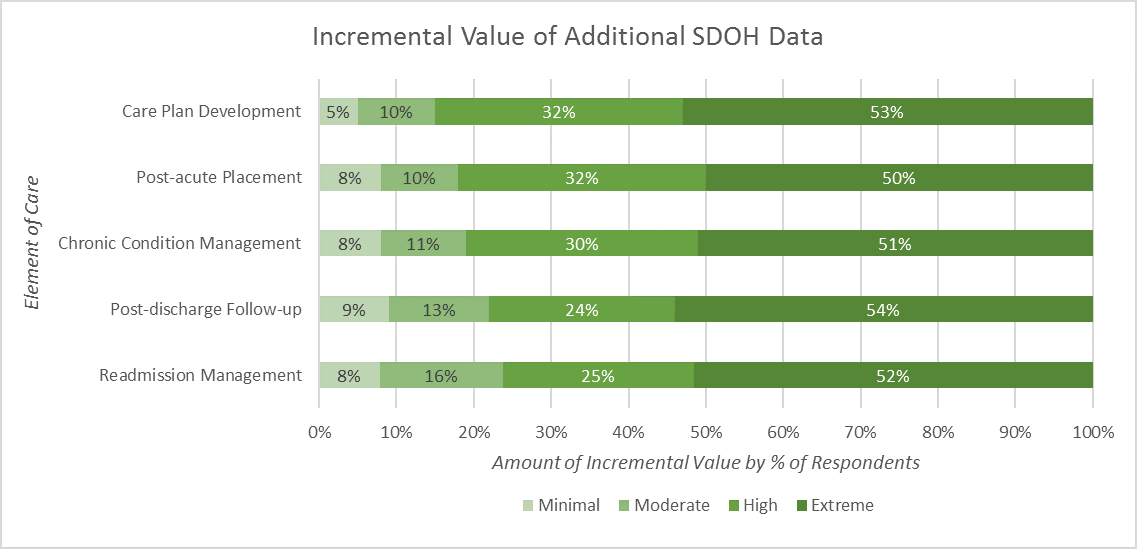
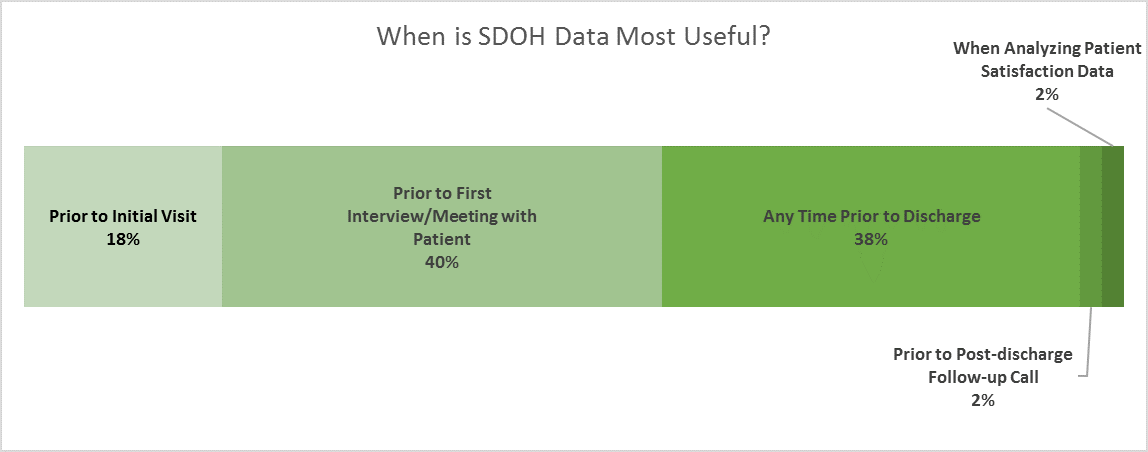
In both fee-based and risk-based environments, this kind of socio-demographic data lacks a direct connection to care programming, and doesn’t surface early enough in the treatment process. What’s needed is patient-level data for every step along the patient’s journey, from care plan development to readmission management and post-discharge follow-up. (see accompanying chart)
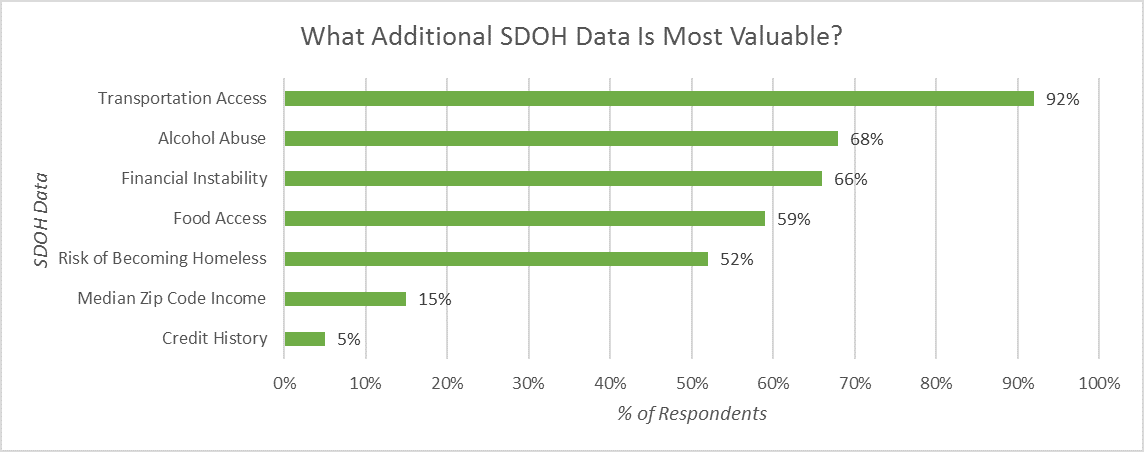
With better patient-specific information, care managers believe they could improve patient experience and outcomes. An overwhelming 92 percent of respondents rated transportation access as one of most useful socio-demographic factors in assessing a patient’s health risk. The most thoughtful, comprehensive care plan will fail if a patient is not able to travel to follow-up appointments or fill prescriptions. Other most-desired socio-demographic data elements were related to alcohol abuse, financial instability, access to healthy food and risk of becoming homeless.
Care teams can use this incremental data to improve their ability to stratify patients based on risk and need, match patients with the right programs and resources, and help care managers respond to patient risks and challenges they may not have been willing to share.
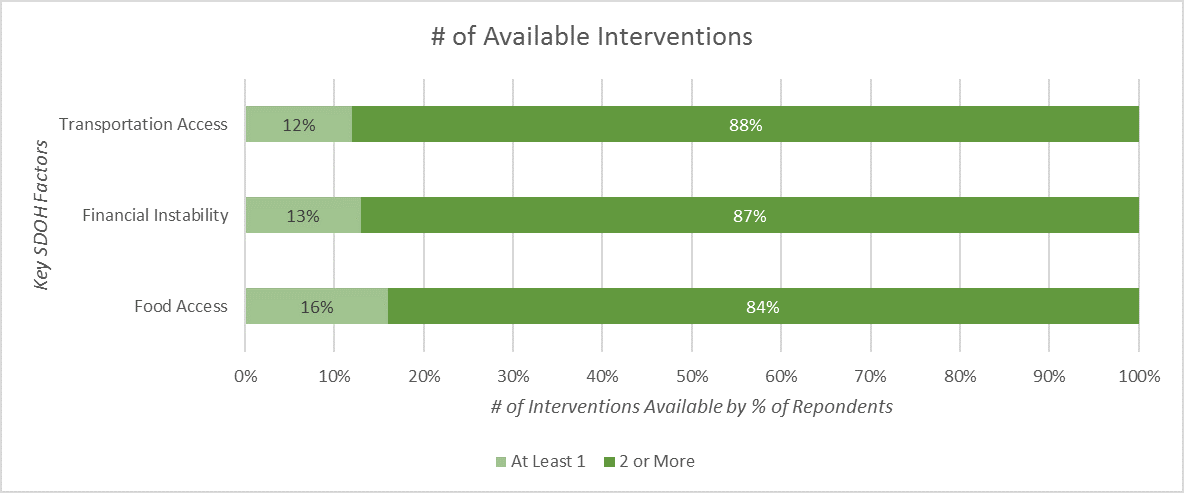
Interestingly, most, care managers indicated they already had many programs in place to make a meaningful impact. Of respondents, 88 percent said they had 2 or more programs available to mitigate transportation risk, 87 percent reported 2 or more programs available to mitigate financial challenges and 84 percent had 2 or more programs available to mitigate food access challenges. But what’s missing is a way to match patient to resources.
...Introduced at the right time
Ideally, social determinant information is available before or immediately upon patient arrival. In many applications, these data points will drive a worklist, as a variable to sort a phone list or to prioritize social work consults. In other situations, early access means more preparation and resource readiness. More than half (58 percent) of survey respondents believed that it would be most helpful to capture and review SDOH data prior to the case manager or social worker interviewing the patient for the first time. They can be informed of issues and challenges going into the patient discussion, and be more targeted in their evaluation to help avoid situations where patients are not forthcoming about their challenges.
...Bends the cost curve for all
Using the right socio-demographic data to proactively identify the risk factors that negatively impact an individual’s health status, and engage them with the appropriate services and resources prior to an acute episode or need for emergency care, is critical to bending the cost curve while simultaneously improving clinical outcomes.
About Connance
Connance is the industry’s premier source of predictive analytic technology solutions that enable providers to optimize financial and clinical workflows for sustained performance improvement.
The views, opinions and positions expressed within these guest posts are those of the author alone and do not represent those of Becker's Hospital Review/Becker's Healthcare. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them.