Total cost of ownership for electronic health record platforms is often addressed as a five- or seven-year figure. But a shift is taking place, as more hospitals and healthcare systems find better TCO planning and return on EHR investment with a 10-year forecast.
The Valley Hospital in Ridgewood, New Jersey, took this decade-long TCO approach when it began to reevaluate EHR platforms in 2012, when challenged with a decision of migrating to the newest platform with their current vendor or selecting a solution from a different vendor. For Vice President for Information Systems and Chief Information Officer Eric Carey, reviewing options for 10 years makes sense for an investment in the double-digit millions.
"We felt no one should be replacing an EHR platform in less than 10 years unless a catastrophe happens," Carey said. "Also, probably the most expensive part of an EHR project is the army of consultants, staff and project managers you need to have to pull everything together. Our implementation has involved 20 FTE over at least one year. Most organizations can't afford to do that more than once every 10 years, and shouldn't have to if the solution they choose is maintained and upgraded well."
Return on staff investment is a good argument for 10-year TCO at the organizational level. Compelling healthcare industry trends also support this new TCO measurement on broader scale:
- Meaningful Use Stages 2 and 3 are affecting health systems and providers this year. These final stages set incrementally higher bars for what's considered Meaningful Use, and health systems need a reliable and budgeted-for EHR as they implement new guidelines.
- The Affordable Care Act is changing how healthcare providers are funded, shifting from services provided to the patient-perceived value of care. As care systems transition to this new funding design in the next few years, unexpected EHR costs can cripple budgets.
- Mergers and acquisitions – of both health systems and EHR vendors – are forever changing the healthcare landscape. In the past two years, HIMSS' Leadership Survey marked a 10 percent increase in healthcare organizations' focus on sustained financial viability, standing at 25 percent in 2014 compared to 15 percent in 20121. To preserve health systems, leaders must avoid as many unexpected costs as possible, especially related to their EHR investment.
There are dozens of lines in any EHR budget, but three in particular can affect the balance of that budget: 1) software maintenance fees and hardware updates, 2) FTE support needs, and 3) the completeness of the EHR software solution. Organizations can better plan for their financial future and success by understanding how these affect TCO.
Factor 1: Software maintenance and hardware updates
Software maintenance fees are a fixed, monthly cost that are calculated as a percentage of the software product fee. Each of the major EHR vendors clearly define these fees and what services are included, although fees vary. The following table demonstrates the difference software maintenance fees can make to TCO, if the original product fee was $2 million.
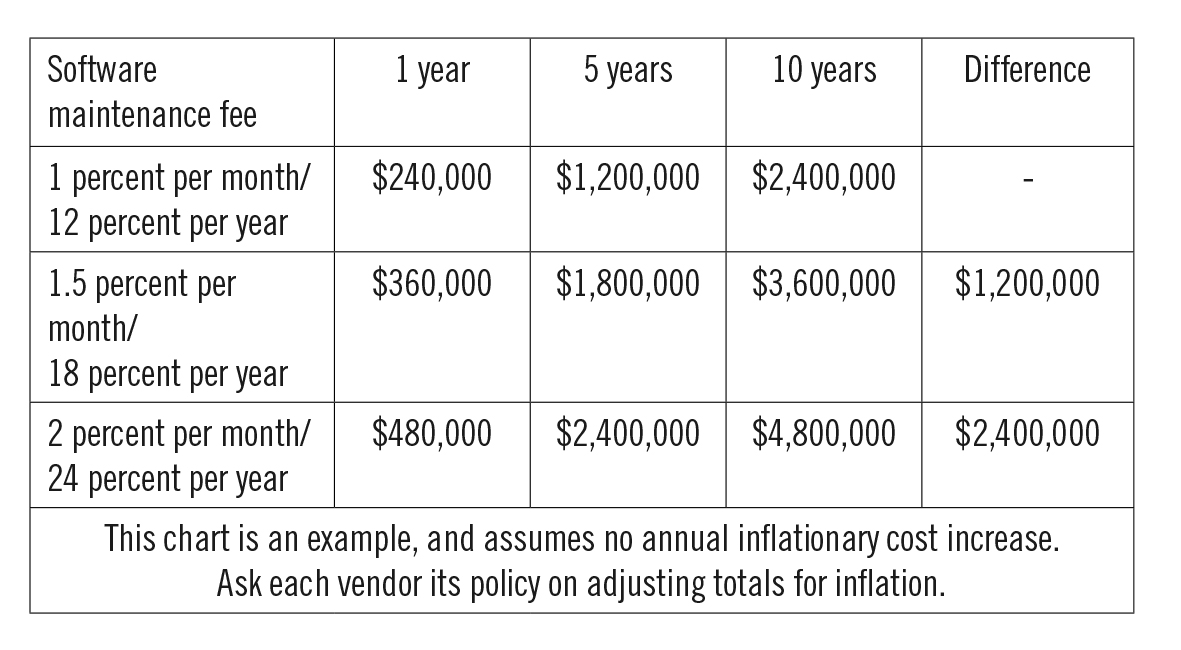
To help make the best decision for your organization and staff, ask each vendor what is included in the software maintenance package. Most include around-the-clock remote support, as well as a dedicated account manager to traffic requests on the vendor side.
Many organizations will update hardware to take full advantage of a new EHR, which also affects 10-year TCO. Hospitals need agile technology and financial strategies to respond to regulatory, clinical and user needs. Take as an example the changing storage capacity requirements for records retention under the American Recovery and Reinvestment Act.
Technology leasing is a good option for hospitals who want maximum agility when responding to these changing IT infrastructure needs. Leasing allows the cost to be spread over time, instead of replacing hardware every three to five years as a large lump sum of capital. Payments are the same each month and technology can be upgraded as needed to meet ever-changing guidelines.
Factor 2: FTE staff support
Staffing and training for EHR solutions has proven a pitfall for many organization budgets. MaineHealth recently announced it will spend $55 million more on its EHR system, mostly for staff training.2 The University of Arizona Health Network added $32 million to implementation, in part for staff training and support.3
With the following best practices, organizations can better estimate their long-term EHR staffing needs.
Best practice #1: Pinpoint staffing trends related to EHR.
The top three EHR staffing needs are implementation, operation and maintenance. Most EHR vendors offer guides and recommendations to help successfully staff its solution.
Implementation traditionally requires the most resources because every person who comes in touch with the technology needs the proper training for their job responsibilities. To alleviate some stress on the IT department, organizations should develop a superuser group. These highly trained employees from across the organization mitigate smaller problems and questions that might arise, and funnel larger requests to the IT department. After implementation, EHR FTE needs decrease and staffing becomes a long-term consideration.
Carey said it's important to remember that an organization still needs to work on its old platform even as training pulls staff time toward the new system. This means backfilling positions across the organization and different departments to still maintain quality of care. Hundreds of positions could need to be backfilled, which takes a large quantity of space and time, and payroll.
Best practice #2: Set aside funds each year for staff training.
For the same reasons that preventative care can help patients avoid larger hospital bills in the future, regular training can help hospitals and health systems avoid unexpected, long-term expenditures.
When looking for an EHR vendor, ask about ongoing training offerings and if there are additional costs to train new employees. Some vendors may include annual on-site seminars, or host on-site training sessions for a fee. Also look for vendor-hosted regional conferences, which serve as a hub of both education and troubleshooting.
Knowing which opportunities exist, a hospital can allocate a certain percentage or dollar amount of the annual EHR budget to training. A hospital can seek board approval for training one time instead of annually by including each year's training expense in the original 10-year contract to be approved.
Best practice #3: Plan for space and time demands.
It rests on the shoulders of the hospital or healthcare system to supply space and equipment, plus travel as needed, for staff training. Carey said those requirements are easy to lose sight of, amid overall space and time demands for staffing and implementing an EHR.
At The Valley Hospital, organizing training was a serious project management undertaking; the organization had to create an off-site location to accommodate training for its 5,000 employees. To budget these costs, organizations should create a training bucket that incorporates any renovation, leasing, equipment and travels expenses, plus payroll dollars, for this expense.
Factor 3: The software solution: Completeness and updates
The completeness of an EHR software solution has one of the longest-lasting effects on long-term TCO, and should be considered from the first meeting through signing a contract. Each vendor offers a different suite of software solutions, which may or may not include third-party applications.
Carey said The Valley Hospital knew from past experience how costs could spiral upward with each additional software system or interface, between contracts and upgrade cycles, and support staff. It set the comprehensiveness of the EHR software as a top criteria in its final decision, to better control the number of vendors and associated costs.
EHR vendors should outline which applications are involved in their proposed solutions. To guard against unanticipated expenses, ask how an EHR vendor works with third parties, and if third-party costs are included in the proposal and estimate. If they aren't, understand how those costs are billed and may change over time.
These questions can help you dig deeper into each vendor's software solution:
- What applications does the EHR vendor provide?
- For services/applications not included, is there a preferred third-party vendor?
- What is the cost for that third-party service? Is that included in the quote you already provided? If not, what is the partner's fee schedule?
- Do you handle communication and coordination with the third party? If so, is there a fee?
Two scenarios, and additional costs, could crop up if an EHR vendor eventually chooses a different third party for an application. In one scenario, your organization may be required to switch third-party vendors, resulting in new software fees and training costs. In the other scenario, you may be able to stay with the current third-party vendor but need additional infrastructure and support to connect with the EHR. These situations should be outlined in the contract, but a contingency fund is also beneficial.
Conclusion
With the convergence of Meaningful Use, the Affordable Care Act, and mergers and acquisitions, care systems should consider the 10-year TCO of their EHR platform to help improve their organization's stability and longevity. By investigating staffing needs, the EHR software solution, software maintenance fees and technology leasing for infrastructure needs, hospitals can better estimate TCO to avoid unexpected costs.
Brad Swenson is senior vice president and chief product strategy and business development officer for Winthrop Resources Corporation, a wholly owned subsidiary of TCF Financial Corporation. Winthrop Resources Corporation provides strategic technology financing, equipment financing and asset lifecycle management services, specializing in healthcare, higher education and professional services industries.
Footnotes
1- 25 Annual HIMSS Leadership Survey. (Feb. 24, 2014). Healthcare Information and Management Systems Society (HIMSS). Retrieved from http://himss.files.cms-plus.com/FileDownloads/2014-HIMSS-Leadership-Survey.pdf
2- Lawlor, J. (Dec. 24, 2013). MaineHealth increasing spending on software system that was involved with billing glitches. Portland Press Herald. Retrieved from http://www.pressherald.com/2013/12/24/mainehealth_increasing_spending_on_software_system_was_involved_with_billing_glitches_/
3- Murphy Ph.D., K. (June 2, 2014). Arizona health system in the red after Epic EHR adoption. EHR Intelligence. Retrieved from http://ehrintelligence.com/2014/06/02/arizona-health-system-in-the-red-after-epic-ehr-adoption/
The views, opinions and positions expressed within these guest posts are those of the author alone and do not represent those of Becker's Hospital Review/Becker's Healthcare. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them.