Case management, with its standards of practice of patient advocacy and resource stewardship and its role as a liaison between patients, payors and the healthcare team, is in a unique position to support the revenue cycle and bridge the gap between a hospital's finance and clinical departments. Hospitals and health systems are facing many financial pressures, including those brought on by the implementation of Recovery Audit Contractor review and denials and the Value Based Purchasing Program outlined by CMS. Many, if not most, hospitals have already experienced RAC denials. Criteria that are measured by VBPP for the process of care have recently expanded to include readmissions. If VBPP is found to be effective in improving quality and reducing costs, additional measures will most likely be added to the CMS program, and commercial payors are developing their own programs. All of this translates into opportunities for case management departments to demonstrate their value within the revenue cycle process.
Utilization management
Utilization management requires that the payor receives timely clinical reviews of inpatient care and that the reviews contain sufficient information for the payor to make a determination of medical necessity and consequently approve the inpatient stay for payment. In cases where there may be disagreement about medical necessity, effective case managers will facilitate discussion between the physicians caring for the patient and the payor's medical director. In addition, case managers can help to identify patients classified incorrectly as observation or inpatient status and collaborate with physicians to rectify the status according to hospital and regulatory policies.
Discharge planning
Timely and appropriate discharge planning facilitates patient transition to the next level of care and helps to avoid unnecessary extension of the length-of-stay. Unnecessary days can translate to denials of care and a lengthy and frequently unsuccessful appeals process, extending the days in accounts receivable. Case management departments are also responsible for appealing post-billing denials for medical necessity.
Care coordination
Care coordination facilitates care progression and ensures that the inpatient stay is not extended unnecessarily. The case manager coordinates care with the physician, the hospital healthcare team, the health plan case manager and others to ensure that care is appropriate and progresses according to the medical treatment plan. Care coordination also includes discharge follow-up to ensure that services such as home healthcare and medical supplies are delivered. This type of follow-up assists in preventing unnecessary readmissions in the event that the patient is experiencing difficulties or services have not been delivered.
Pre-admission phase
The pre-admission phase incorporates all of the activities that occur in the outpatient setting or admissions process prior to the patient arriving in the hospital bed. This would include the activities that occur in the emergency department, admitting office/patient registration and patient bedding process, etc. Look for the following characteristics:
Admission phase
Critical case management functions during the admission phase include admission review for medical necessity and appropriate patient class using standardized inpatient utilization criteria. Case management activities in alignment with the revenue cycle include:
Concurrent phase
The concurrent phase of hospitalization is a busy time for case managers. During this phase, case managers are conduits of communication with physicians, the hospital healthcare team, the patient and family members, the health plan CM, post-acute providers and community resources. At the same time, they are reviewing the patient's clinical status and progress, documenting their case management plan and interventions, identifying barriers to advancing the medical treatment plan and discharge plan and implementing a plan of action to address these barriers. Alignment with the revenue cycle during this phase includes:
Discharge phase
The discharge phase of hospitalization is an area of focus addressed in many of the Transitions of Care projects. National Transitions of Care Coalition, The Joint Commission and legislation mandating healthcare reform have highlighted the need for clinicians across the continuum of care to communicate with each other as hand-offs occur. Improving care transitions has an obvious effect on the quality of care and now, with the advent of the VBPP, quality measures will have a financial component as well. Case management programs featuring early discharge planning and assertive utilization management demonstrate the following:
Post-discharge phase
The post-discharge phase of hospitalization continues to highlight important activities for case management. Prompt attention to payer requests for retrospective reviews, providing discharge reviews and any additional clinical information required for authorizing inpatient days and follow-up on post-billing denials have a direct impact on the revenue cycle. Case management follow-up with targeted patient populations (e.g. those with readmissions, frequent ED visits or those with chronic diseases) may help to decrease readmissions and improve patient and physician satisfaction. Key case management activities in the post-discharge period that impact the revenue cycle include:
The financial pressures on hospitals introduced by the economy and healthcare reform cannot be ignored. Ensuring that your case management department is a powerful resource and ally in supporting the revenue cycle is a vital approach for success.
Kathleen Miodonski is a manager at The Camden Group, with over 16 years of experience in case management and utilization management in hospitals and health plans. She has successfully led case management departments through model redesign and implementation and has extensive expertise in hospital operations, managed care, and disease/utilization/case management.
Structuring Hospital Service Line Management for Success
Case management responsibilities in relation to the revenue cycle
The typical case management department is responsible for utilization management, discharge planning and care coordination, and these functions all relate to the revenue cycle.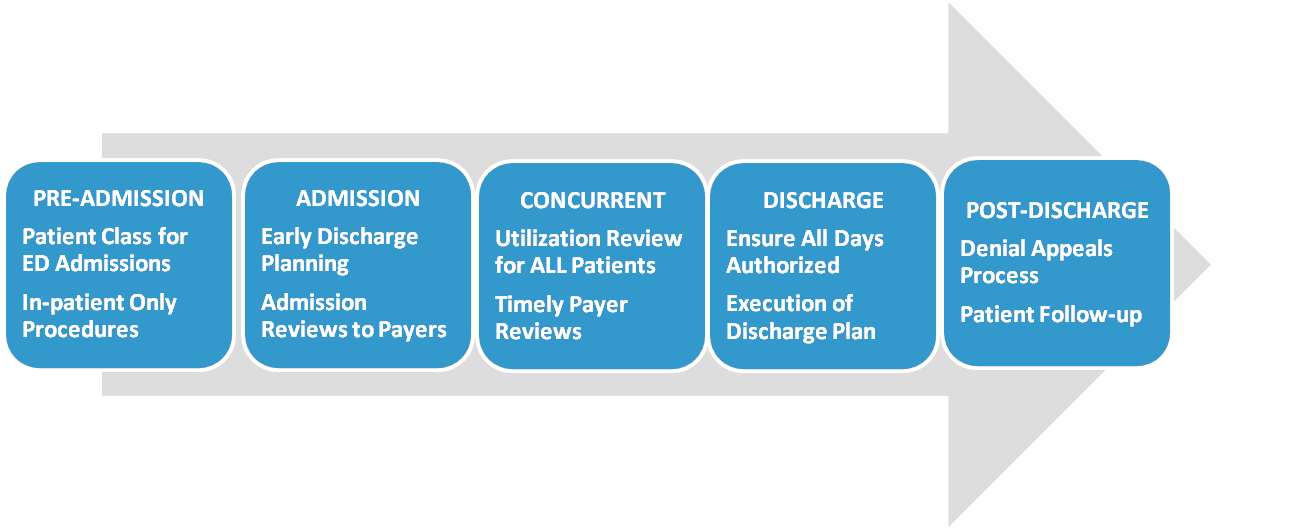
Utilization management
Utilization management requires that the payor receives timely clinical reviews of inpatient care and that the reviews contain sufficient information for the payor to make a determination of medical necessity and consequently approve the inpatient stay for payment. In cases where there may be disagreement about medical necessity, effective case managers will facilitate discussion between the physicians caring for the patient and the payor's medical director. In addition, case managers can help to identify patients classified incorrectly as observation or inpatient status and collaborate with physicians to rectify the status according to hospital and regulatory policies.
Discharge planning
Timely and appropriate discharge planning facilitates patient transition to the next level of care and helps to avoid unnecessary extension of the length-of-stay. Unnecessary days can translate to denials of care and a lengthy and frequently unsuccessful appeals process, extending the days in accounts receivable. Case management departments are also responsible for appealing post-billing denials for medical necessity.
Care coordination
Care coordination facilitates care progression and ensures that the inpatient stay is not extended unnecessarily. The case manager coordinates care with the physician, the hospital healthcare team, the health plan case manager and others to ensure that care is appropriate and progresses according to the medical treatment plan. Care coordination also includes discharge follow-up to ensure that services such as home healthcare and medical supplies are delivered. This type of follow-up assists in preventing unnecessary readmissions in the event that the patient is experiencing difficulties or services have not been delivered.
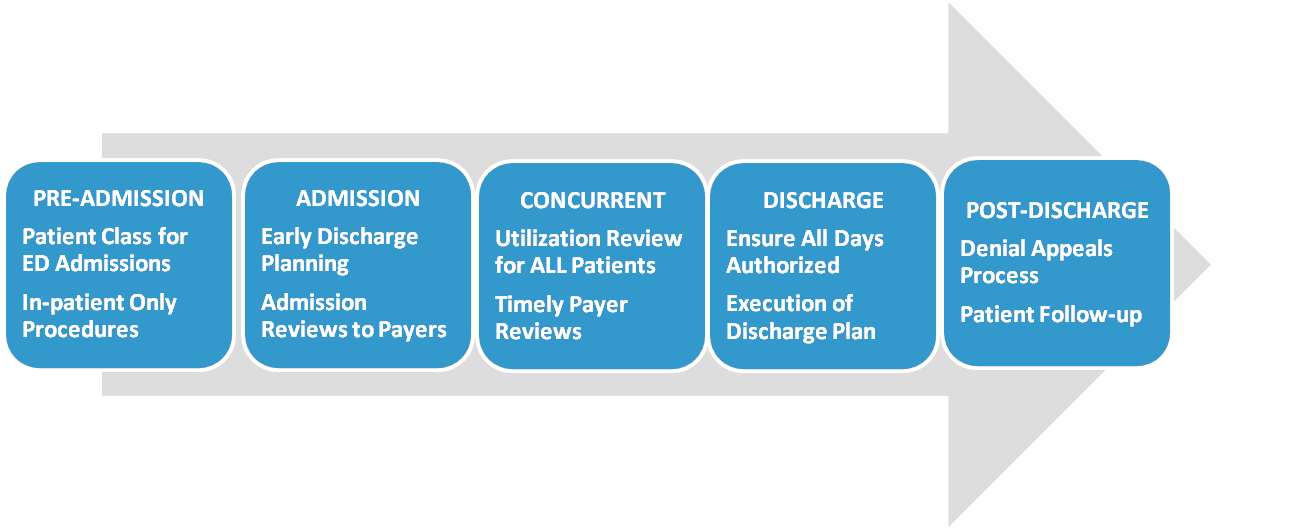
Case management and revenue cycle alignment
The acute care, inpatient experience can be divided into five phases: Pre-Admission, admission, concurrent, discharge and post-discharge. Certain case management activities associated with each of these phases impact the revenue cycle. In addition, there are at least two other areas — health plan contracting and the hospital's utilization management committee — that require active case management participation to yield the best clinical and financial outcomes. The following describe characteristics and case management activities hospitals should see in each phase if case management is successfully aligned with the revenue cyclePre-admission phase
The pre-admission phase incorporates all of the activities that occur in the outpatient setting or admissions process prior to the patient arriving in the hospital bed. This would include the activities that occur in the emergency department, admitting office/patient registration and patient bedding process, etc. Look for the following characteristics:
- Elective surgery review for Medicare "inpatient only" procedures. Many commercial payors have adopted this list as well. Incorrect patient classification for "inpatient only" procedures delays payment in the best case scenario and can result in a denial of payment in the worst. Errors at the front end require staff in case management and finance/billing areas to take time to correct what could have been done correctly in the first place.
- ED screening for admission to alternate level of care versus hospital admission. Inpatient care that could be provided at a lower level of care is most likely to be denied by payors, inappropriately consumes hospital resources and exposes patients to all of the risks of hospitalization such as infection, falls, etc.
- ED review for correct patient classification (inpatient versus observation). As with the Medicare "inpatient only" list, incorrect patient classification for hospital admissions will result in delay or denial of payment and consume valuable staff resources to rectify.
Admission phase
Critical case management functions during the admission phase include admission review for medical necessity and appropriate patient class using standardized inpatient utilization criteria. Case management activities in alignment with the revenue cycle include:
- Providing clinical reviews to payors for urgent/emergent admissions. Case managers provide the health plan with clinical admission reviews required according to payor contracts and the clinical reviews at the time of admission for the inpatient stay.
- Admission review of elective admissions. Even if the elective surgical procedure has been pre-certified by the payor, changes in patient condition following surgery or procedures will necessitate the case manager to review and follow-up with the health plan.
- Early identification of discharge needs. The relationships between discharge planning and transitioning to VBPP, prevention of readmissions, hospital acquired infections, and patient safety goals have already been well highlighted in literature. In terms of the revenue cycle, early discharge planning prevents extended LOS, avoidable inpatient days and denials. While many organizations talk about early discharge planning, the question to answer is: What specifically is the process in place that ensures discharge planning truly begins at admission (or even pre-admission for elective procedures)?
Concurrent phase
The concurrent phase of hospitalization is a busy time for case managers. During this phase, case managers are conduits of communication with physicians, the hospital healthcare team, the patient and family members, the health plan CM, post-acute providers and community resources. At the same time, they are reviewing the patient's clinical status and progress, documenting their case management plan and interventions, identifying barriers to advancing the medical treatment plan and discharge plan and implementing a plan of action to address these barriers. Alignment with the revenue cycle during this phase includes:
- Application of utilization management criteria such as InterQual or Milliman Care Guidelines to all inpatients. While most case managers understand the need for utilization review for commercial payors, many departments do not perform utilization review on Medicare and/or Medicaid patients because concurrent reviews are not "required." Consequently, opportunities to identify inappropriate admissions or unnecessary hospital days are missed. This results in extended LOS and increases the risk of commercial and RAC denials.
- Provide timely concurrent continued stay reviews for payers and take appropriate action when criteria not met. This may seem obvious, but many case management departments are faced with two fundamental issues in fulfilling this requirement. First, there is no way to monitor outstanding reviews or those not completed in real time. Second, case managers are often passive when utilization criteria is not met. Missed reviews prolong the revenue cycle, and passive case managers result in extended LOS and increase the probability of denials.
Discharge phase
The discharge phase of hospitalization is an area of focus addressed in many of the Transitions of Care projects. National Transitions of Care Coalition, The Joint Commission and legislation mandating healthcare reform have highlighted the need for clinicians across the continuum of care to communicate with each other as hand-offs occur. Improving care transitions has an obvious effect on the quality of care and now, with the advent of the VBPP, quality measures will have a financial component as well. Case management programs featuring early discharge planning and assertive utilization management demonstrate the following:
- Final review of authorized days. Claims submitted for inpatient stays must have all days authorized for medical necessity or there will be delays in payment. Some health plans may require the hospital to go through the appeals process if the patient is discharged before all inpatient days have been authorized, thus delaying payment. The ability to determine that all inpatient days for all patients have been authorized is the key to avoiding delays in payment for unauthorized days.
- Execute the discharge plan. Discharge plans that are not comprehensive and do not incorporate best practices may result in readmissions. Patients readmitted with diagnoses targeted by the VBPP will have a negative effect on revenue.
Post-discharge phase
The post-discharge phase of hospitalization continues to highlight important activities for case management. Prompt attention to payer requests for retrospective reviews, providing discharge reviews and any additional clinical information required for authorizing inpatient days and follow-up on post-billing denials have a direct impact on the revenue cycle. Case management follow-up with targeted patient populations (e.g. those with readmissions, frequent ED visits or those with chronic diseases) may help to decrease readmissions and improve patient and physician satisfaction. Key case management activities in the post-discharge period that impact the revenue cycle include:
- Active denials management and timely response to post-billing denials and outstanding reviews. While the goals of any case management program include prevention of denials, post-billing denials for medical necessity cannot be entirely eliminated. A successful appeals program will decrease days in AR and write-offs and enhance revenue.
- Follow-up with patients with discharge plans including home care and durable medical equipment. Follow-up contact for patients with complex discharge needs is an established best practice and may decrease readmissions. Patients readmitted with diagnoses targeted by the VBPP will have a negative effect on revenue.
- Follow-up with skilled nursing facilities. Follow-up contact for patients with complex discharge needs is an established best practice and that may impact readmissions. Patients readmitted from SNFs to acute care within 30 days that are targeted by the VBPP will negatively impact revenue.
Strategies for aligning case management processes with revenue cycle and organizational goals
The case management department for a hospital should serve to integrate the clinical and financial goals for the organization. Key strategies for aligning a case management program to the revenue cycle include examining staffing performance, processes to maintain current education in case management principles, program goals and outcomes measurement and interdepartmental relationships — especially with finance. Additional strategies for finance leaders to undertake include:- Lobby to ensure that there is case management representation in key organizational functions and initiatives, particularly in health plan contracting. To successfully develop an organization's processes, consideration should be given to the resources and experience case management can offer. This is especially important in health plan contracting. Case managers can serve as an "early warning system;" case management staff has daily contact with payers and can provide valuable insight into health plan policies and practices that may have a negative impact on hospital operations and finances.
- Participate in addressing knowledge, data capture and training deficits in relationship to the revenue cycle within case management leadership. Case management leaders in the era of healthcare reform must recognize challenges and opportunities for the organization and develop the case management program accordingly. Current case management leaders must have the skill to lead the staff effectively and assure that relevant data is available through the change process. CFOs should meet regularly with case management leaders and provide formal and informal mentoring regarding the revenue cycle.
- Support the budget to ensure the appropriate infrastructure available to case management, which in turn supports the goals of the organization. Leveraging technology can improve the efficiency of staff. Use of cell phones to facilitate communication with internal and external contacts and computer programs that support the workflow and allow for real-time monitoring of work status will allow case managers to improve productivity. Monitoring productivity in key areas such as completion of payor clinical reviews will assist managers in deploying staff and ensure that they focus on the "right" things in utilization management. Support from the finance department helps ensure that the case management has the infrastructure needed.
- Ensure finance representation and participation in the hospital's utilization management committee to support case management processes and system-wide process improvement. The finance department should provide reports on metrics such as cost per case, LOS, ancillary costs per case and denials data. Case management should contribute reporting on denials rates, overturned denials for medical necessity and potentially avoidable days. Potentially avoidable days' reporting identifies quality and efficiency occurrences that may affect LOS. The identification of a root cause and resolution of the avoidable day issue may require the support and cooperation of multiple departments and areas across an organization. Potentially avoidable days can affect throughput and prevent or delay new admissions from entering the hospital.
- Clearly identify how denials management responsibilities and accountabilities are divided between finance and case management. Case management is typically responsible for medical necessity denials. However, medical necessity denials frequently encompass aspects of coding and billing. Collaborative processes must be developed between the finance and case management departments. The overall program must allow the appropriate amount of time and training for staff in both departments to address denials and appeals successfully. These accountabilities can be incorporated into job descriptions but without proper training and adequate time allotted for appeals activities, the appeals process will not yield the desired outcomes.
- Support the appointment/hiring of an effective physician advisor/medical director in the case management department. An effective physician advisor/medical director lends credibility and authority to the case management department and core process activities. The Medicare Conditions of Participation for Hospitals requires that physician members of the utilization review committee make the final decision regarding medical necessity of inpatient admissions and continued inpatient care. Without the support of a physician advisor or a utilization review committee, case managers engaged in utilization review can discuss patients who fail to meet acute-care criteria but would benefit from a physician advisor to engage in a conversation with the primary care provider to resolve the issue. CFOs can help support the appointment by proactively allocating appropriate resources so the organization can recruit and hire the best qualified physician advisor.
The financial pressures on hospitals introduced by the economy and healthcare reform cannot be ignored. Ensuring that your case management department is a powerful resource and ally in supporting the revenue cycle is a vital approach for success.
Kathleen Miodonski is a manager at The Camden Group, with over 16 years of experience in case management and utilization management in hospitals and health plans. She has successfully led case management departments through model redesign and implementation and has extensive expertise in hospital operations, managed care, and disease/utilization/case management.
More Articles From The Camden Group:
From Silos to Service Lines: Integrating Care to Meet Hospital GoalsStructuring Hospital Service Line Management for Success