Hospitals and health systems across the country are experiencing significant pressure to reduce costs and improve quality.
The shift from volume to value continues to accelerate, being driven by regulatory changes such as Bundled Payments for Care Improvement (BPCI), Shared Savings Programs (ACOs), Comprehensive Care for Joint Replacement (CJR), the recently announced bundles for cardiovascular services, and Medicare Access & CHIP Reauthorization Act of 2015 (MACRA).
Most analysts agree that the newly elected Trump administration will not move away from the shift to value. In fact, the newly appointed head of the Department of Health and Human Services, Representative Tom Price, voted for MACRA. And commercial insurers and self-insured employers are beginning to implement value-based programs as well.
While hospitals have made significant strides with their traditional performance improvement efforts, clinical redesign, including clinical variation reduction, has emerged as the next frontier of performance improvement. Redesigning care and eliminating clinical variation are critical not only to ensuring patients receive the safest, highest-quality care, but also are integral components of reducing the overall cost of healthcare — on both the national and individual hospital level.
DCH Health System has implemented clinical redesign efforts that have reduced clinical variation and standardized key care processes to best practices, generating a myriad of positive effects. These efforts have led to higher engagement among physicians and engaged leaders, revenue enhancement, reduced costs and, most importantly, improved quality and safety. As the industry shifts from volume- to value-based reimbursement models, these benefits are fundamental to thriving in a new healthcare era.
From recent initiatives to reduce clinical variation within DCH Health System, there have been lessons learned and best practices identified that made the implementation of the clinical redesign program highly effective. While the complexity of clinical redesign initiatives should not be underestimated, these five principles can help hospital and health system executives to navigate the process within their own organizations.
1. Engage Medical Staff
Physician leaders and executive leadership must formally and informally engage the medical staff to communicate their expectations, goals, measures and accountability for the results of the clinical redesign effort. Hospital leadership must also put in place processes that ensure physician-directed communications, listening and real involvement in identifying, measuring and reducing variation. This includes participation in interdisciplinary rapid design teams for high-volume diagnosis-related groups (DRGs) or service lines to review data and understand current practice variation by physicians. Trustworthy, risk-adjusted data analytics can provide insights for medical staff regarding their variation in resource use such as diagnostics, pharmaceuticals and other professional resources. Administrators and medical staff leaders will be most successful when they partner in a style that is (1) supportive and collaborative, (2) creates the vision but is not directive, and (3) rewards those who are engaged and achieve the required outcomes.
2. Ensure Relevant and Accurate Data
Risk-adjusted, physician-specific clinical variation data form the foundation for engaging physicians to reduce clinical variation. Capturing and sharing these analytics allows clinical teams to understand the severity of illness of each practitioner's patient population, thus removing the concern that one physician's patients are more complex than others. Risk-adjusted analytics also reduce physician resistance and further physician buy-in to study and reduce variation. It's important that clinicians and the entire improvement team receive updated analytics on a frequent and predictable basis in order to see reductions in variation and support changes in behavior.
3. Create True Interdisciplinary Care Delivery
To create a culture of interdisciplinary collaboration with an eye toward innovation, best-practice and early adoption, organizations must build interdisciplinary teams that encourage cross-functional discovery of opportunities to improve patient care outcomes. Regulatory bodies, such as Centers for Medicare and Medicaid Services (CMS), the Agency for Healthcare Research and Quality (AHRQ), and the Health Resources and Services Administration (HRSA) are holding organizations and clinicians responsible for interdisciplinary collaboration with a goal of patient safety and clinical outcomes. Courageous leadership across all disciplines can ensure a culture of collaboration and the transparent flow of information. In clinical redesign, this transparency should be reflected in communication and hand-offs between clinicians and patients, between clinicians themselves, between healthcare organizations and the public, and among healthcare organizations as a whole. This successful communication facilitates the timely progression of care and safe transitions to the least restrictive venue of care.
4. Utilize Scorecards and Dashboards
Both blinded and unblinded physician scorecards that measure improvement in targeted metrics serve as an important tool in demonstrating progress. We recommend providing refreshed data on a monthly or quarterly basis (depending on the metric) so that improvement teams can evaluate the impact of initiatives and continue to adjust improvements in a timely fashion. Dashboards represent a fundamental component of clinical redesign programs. They allow the medical staff, healthcare team and board to evaluate the success of their efforts against the goals defined, track trends, and identify opportunities for improvement. An effective dashboard should include core process and outcome metrics that reflect the goals of the program, provide an overview of program effectiveness, and have relevance to the various disciplines on the team. Moreover, the data chosen should reflect clinical, quality, and financial considerations.
Process measures such as discharges to home care and skilled nursing, follow-up phone calls, and ancillary involvement, may also correlate to the clinical data. Patient satisfaction scores and average scores from self-reported wellness surveys are quality measures that can round out the scorecard and document success.
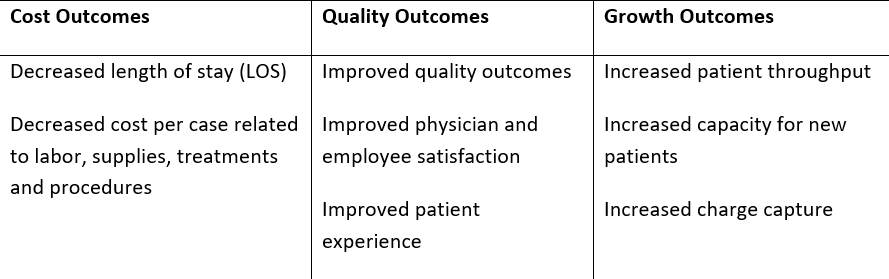
Sample Outcomes from Defined Metrics
5. Focus on Quality and Patient Satisfaction
Implementing clinical redesign and reducing clinical variation can impact several key metrics that are critical to improving the quality of care delivery. Working with clinicians to implement a care delivery process that eliminates unnecessary care and is aligned with best practices often results in improvements to key quality indicators such as readmission and complication rates. Additionally, standardization of certain aspects of care delivery results in a more predictable care pathway, which enables providers and staff to manage patient expectations, enhances patient satisfaction and ultimately delivers more optimal care. Patient education is a critical aspect of meeting the ever-increasing expectations of the level of satisfaction of patients and their families. To ensure optimal satisfaction, patients should know prior to, or early upon admission when to expect to be discharged so planning by the family can take place. Patient education related to the plan of care and/or pathway should inform the patient and family throughout the care progression.
Today's hospitals and health systems are not alone in facing the changes of the evolving healthcare landscape. While each healthcare organization has unique challenges and opportunities on their journey to reducing clinical variation, they can guide their efforts by examining other organizations' strategies and by enlisting experienced professionals who are knowledgeable about the process to ultimately yield improved quality and reduced costs.
The views, opinions and positions expressed within these guest posts are those of the author alone and do not represent those of Becker's Hospital Review/Becker's Healthcare. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them.
