On March 31, Congress passed a bill to address the sustainable growth rate for physician reimbursement, which also included language to delay the ICD-10 implementation date by at least one year. After a month of uncertainty, CMS released a statement on May 1 announcing they expect HHS to release an interim final rule in the near future that will include a new compliance date that would require the use of ICD-10 beginning on Oct. 1, 2015.
The industry now has a new implementation date, which is a step in the right direction. However, healthcare organizations are left "holding the bag" in terms of assessing and understanding the impact on their respective organizations, members and partners. Industry experts estimate this delay will cost between $1 billion and $6 billion.
The industry consensus thus far indicates little or no stopping in the implementation efforts for ICD-10. In fact, electronic medical record vendors are encouraging customers to move ahead with implementing ICD-10 terms and tools this year. This will help improve clinical documentation specificity. It will also give physicians more time to adjust to the ICD-10 documentation concepts and habitually include these in their notes prior to the revised compliance date.
Use the gift of time wisely
It's important for organizations to take a step back and understand how this new deadline impacts stakeholders. Many of our clients are forging ahead so momentum is not lost and their financial investment is mitigated. We are helping our clients ask important questions now, including the following:
1. What should we continue?
2. What should we slow down?
3. What should we shelve entirely, and when should we restart in order to meet the new transition date?
4. What is the financial impact?
Refining the ICD-10 delivery approach: Focusing on the way forward
We have found that the level of readiness and the impacts of the delay vary widely with each organization. We are assessing the impact across the following functions:
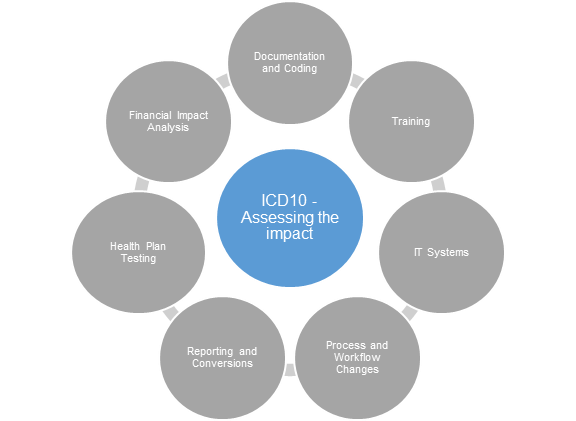
1. Documentation and coding — Continue to work in these areas.
- Move forward with current implementation activities focused on coding and documentation, while continuing to bill in ICD-9 until the new compliance date.
- These activities include establishing or refining a clinical documentation improvement program, dual coding records in ICD-9 and ICD-10, and implementing new tools and processes to improve coder productivity. These investments will lead to better denials management, improved clinical documentation, increased coder productivity and improved financial risk modeling for ICD-10.
2. Training — Adjust efforts to focus on key activities.
- For providers: Focus on related specificity in clinical documentation and those with the greatest reimbursement impact under ICD-9. This allows providers to become familiar with documentation requirements prior to the implementation date and to improve the specificity of clinical documentation for both ICD-9 and ICD-10. Improved documentation practices will have a positive impact on DNFB, A/R days and denials management.
- For coders: Continue dual coding so that coders can practice using ICD-10 and receive feedback to help them improve. Plan for new coder and refresher training in 2015.
- For all other affected roles, align training plans closer to the new implementation date.
3. IT Systems — Use additional time to prioritize work efforts and resource impacts.
- Review the current application remediation schedule to assure priority apps are moved as far forward in the timeline as possible to minimize impacts to staff productivity.
- Keep your application inventory current, coordinate new timelines for changing application software release dates and ensure ICD-9 codes will continue to be accepted/transferred after Oct. 1, 2014.
- Assess whether there are contractual agreements requiring ICD-10 upgrades or enhancements in 2014.
- Analyze internal integration testing efforts to determine what testing should be done now, and what testing should be done closer to the revised compliance date. Are you upgrading your EMR in 2015? Are you replacing or adding new clinical applications? It might not make sense to complete integration testing now, due to the changing IT landscape and key application initiatives already planned for 2015.
4. Process and workflow changes — Improve the foundation of business processes ICD-10 will be built on
- Use the time to standardize and optimize front-end revenue cycle processes, including advanced benefit notifications, pre-authorizations, scheduling and referrals.
- Investing in improved and streamlined front-end processes will provide short-term benefits to denials management and write-offs, as well as minimize the potential impact to ICD-10 down the road.
5. Reporting and conversions — Adjust based on anticipated change in the next year.
- In many cases, clients are moving forward with developing forms, reports, policies and procedures to minimize additional costs resulting from the delay by completing all work, except training and printing, by Oct. 1, 2014.
- In other cases, clients are holding off on remediating reports or file extracts until they get closer to the revised compliance date.
- If the reporting landscape is anticipated to evolve — due to retired or new operational requirements, ancillary applications, or trading partners — focus on maintaining an accurate inventory between now and 2015 and complete all work within a consolidated effort next year.
6. Health plan testing — Contingent upon health plan participation.
- Many large health plans are moving ahead with their efforts and have indicated interest in going forward with integration testing with providers. Discovering functional and technical issues now through testing with health plan partners reduces risk closer to the compliance date.
- For health providers that continue to test: Consider piloting ICD-10 claims with an interested health plan partner in advance of the compliance date to further flush out system and workflow gaps and to ensure operational readiness.
7. Financial impact analysis — Start analysis now.
- Improved documentation and coding affects financials. Compare the results of the dual-coded ICD-10 claims with the ICD-9, and identify where the shifts in expected reimbursement are greatest. Analyze root cause to determine whether improvements to documentation or coder performance can be realized.
- Consider risk to cash flow, and plan to mitigate risks by analyzing the results of ICD-10 coding and health plan partner testing. Where are you seeing increases in denials in the testing?
Focus your team on what matters most to the organization
Organizations should focus on areas that will deliver benefits regardless of the implementation date, such as documentation improvement and coding. Additional focus should concentrate on areas that help reduce risk through ICD-10 financial impact analysis, such as technology remediation and health plan testing.
Terri Mayne-Jarman, Bill Klossner, Erin White and Nate Nelson are healthcare experts with Point B. Point B's healthcare practice supports organizations working on critical challenges in today’s complex marketplace — from healthcare reform to performance management.
More Articles on ICD-10:
CMS: Partial Freeze on ICD-10, ICD-9 Updates to Continue Through 2016
How ICD-10's Latest Delay Affects Students
ICD-10 Staffing Concerns Remain: 6 Questions to Fine Tune Your HIM Budget

