As health systems seek to capture ambulatory services, grow revenue, and prepare for risk-based reimbursement models that favor low-cost care alternatives, many are struggling to find the right leadership structures for their ambulatory enterprise.
It has long been understood ambulatory services are markedly different from inpatient services and require a different operating model to be successful. Consumers and physicians have a different expectation of service, convenience, and efficiency, all of which are difficult to achieve in the ambulatory enterprise with hospital management models geared to delivering complex, customized treatment. As a result, the ambulatory enterprise needs a new leadership and structural model geared towards its specific needs.
A New Type of Leader Needed
To create a successful ambulatory enterprise, health systems need leadership that understands and can improve the key ambulatory success factors: consumer focus, standardized predictable processes, and lean operations.
Consumer focus. In ambulatory services, the consumer's focus is on service and convenience. These are the markers of patient satisfaction more so than clinical outcomes which are expected to be high quality. Take for example an MRI scan. Consumers, all but the most demanding subspecialty physicians, and payers all assume the clinical part of the MRI scan will be the same, no matter where the scan is preformed and read. Moreover, with digital imaging, re-reads are easily completed. As a result, we are seeing dramatic growth in price and convenience competition for MRI. Many simple ambulatory services benefit more from a retail-service model than from a complex clinical delivery model. This consumer and retail focus demands leaders that understand the consumer relationship and retail model.
Standardized, predictable processes. The ability to accurately predict and continually streamline the ambulatory processes requires a high degree of standardization. Expectations for a smooth, predictable process are many times higher in the ambulatory setting than they are in the hospital setting. Consider for example a typical diagnostic test that might take 30 minutes from check-in to completion whereas an inpatient stay at 4.5 days is more than 200 times longer. As a result, a 10-minute variation affects consumer's experience and the operational efficiency much more in the ambulatory setting than the inpatient. This need for standardized, predictable processes means ambulatory services must be run with standardization-hawks that create processes predictable down to the seconds not days.
Efficiency and lean operations. The role of ambulatory services is changing. Ambulatory services were once ancillary to inpatient healthcare delivery model. Today, however, ambulatory services are both a feeder to the inpatient and more often represent the endpoint of the healthcare delivery for the patient. As ambulatory become an endpoint of care, and as ambulatory services grow and represent a larger portion of the revenue, the ambulatory enterprise must be independently financially viable and not depend on downstream contribution to make the business case. However, with smaller total revenue per unit than typical hospital-based care, achieving financial independence is difficult unless processes are highly efficient. This is doubly the case as the hospital-based technical fees are experiencing tremendous downward pricing pressures. In many markets, the hospital-based pricing is over and health systems are finding they must price services at or near the rates offered by freestanding centers owned by investor and physicians. Consider dropping hospital-based MRI net revenue rates from $1,200 commercial net revenue per case to $499 ambulatory rates to compete. In these scenarios, health systems cannot run hospital HR salary or benefits, regulations, overhead, or management without very lean processes.
Leaders with these three skillsets are needed. Unfortunately many health systems have not grown the ambulatory leaders they need. To encourage this growth, new organizational structures are needed.
New Ambulatory Organizational Structures
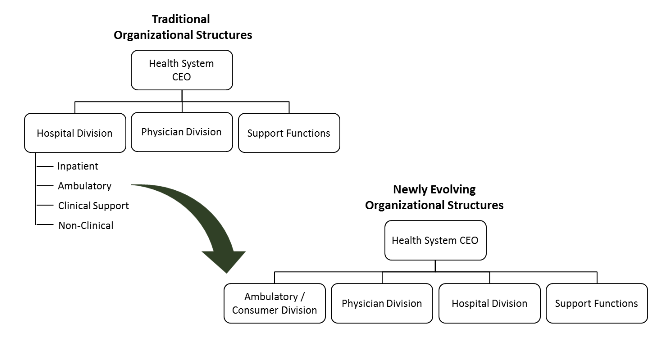
To solve the challenge of building ambulatory management models that address consumerism, health systems are beginning to experiment with creating distinct ambulatory enterprises that are still coordinated with the inpatient and physician enterprises. Freeing the ambulatory enterprise to serve the market with the most effective models brings the threat of cannibalization of hospital volumes but also a responsibility to create a division with independent financially viability. Without some separation, concern about protecting the larger inpatient enterprise stifles the ambulatory enterprise and provides space for competitors to move in with their ambulatory services. When considering ambulatory expansion opportunities, many health systems would do well to heed the saying: "if you don't cannibalize yourself, someone else will."
As a result of these factors, we believe a move towards setting up the ambulatory enterprise as an equal is just beginning and will see most health systems with formal ambulatory enterprise leaders in the coming five years.
The shift of volume towards the ambulatory environment has been a sustained trend of decades that population health reimbursement models will only serve to accelerate. As a result, health systems must focus on developing the new ambulatory leaders needed to effectively advance these operations and create the structures needed to make this growing part of the health system successful.