The bundled payment episode definitions in previous Medicare bundled payment initiatives such as the Medicare Participating Heart Bypass Demonstration and the Medicare Acute Care Episode Demonstration included only services provided during the inpatient stay. As inpatients, these patients are closely monitored by physicians and hospital staff, and receive only services ordered by their attending physicians. The time frames over which the services are provided are generally short, and services are focused on the reason for the patient's admission. In addition, these demonstration projects included only surgical patients within a rather narrow range of diagnoses.
The Medicare Bundled Payment Initiative being implemented in 2012 includes services provided to patients for a period between 30 and 90 days or longer after discharge, under certain models of the program. During this time period patients are no longer under the constant management of their attending physician and may develop conditions, and seek treatment for those conditions, outside of the control (and indeed without the knowledge) of the physicians who were responsible for their inpatient care. Notwithstanding this, the Medicare costs of the services will be charged against the bundled payment budget unless specifically excluded from that type of episode. In the MBPI application, CMS indicated its interest in "understanding how care redesign extends to a beneficiary’s transition back into the community," and therefore the applicant must understand the type of post-discharge care provided and be prepared to manage it effectively.
Time periods in the bundled payment episode
The post-discharge period to be included in the episode can be selected by the applicant, but must be at least 30 days. Applicants selecting a post-discharge period of 90 days or longer have a lower minimum required discount (2 percent) than applicants selecting the shorter period (3 percent discount).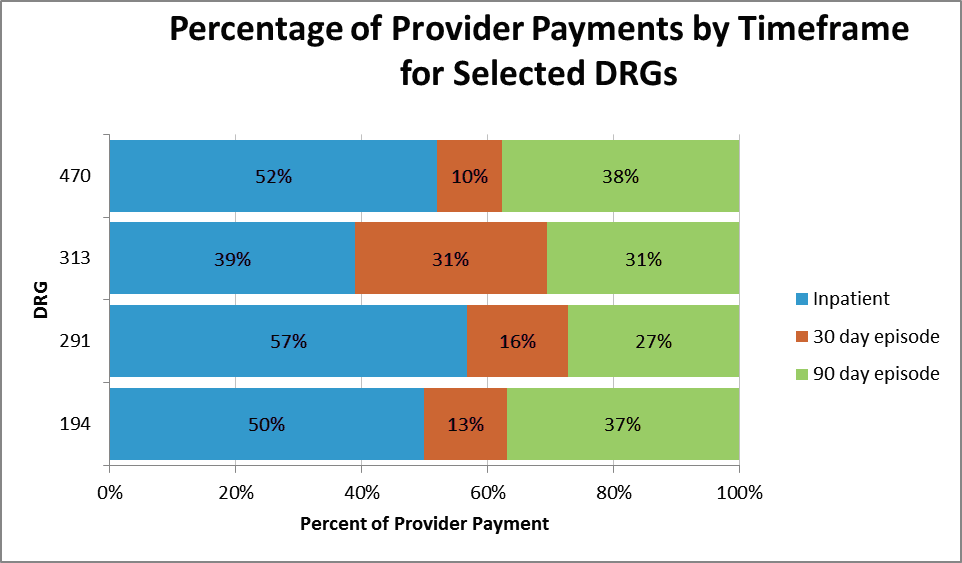
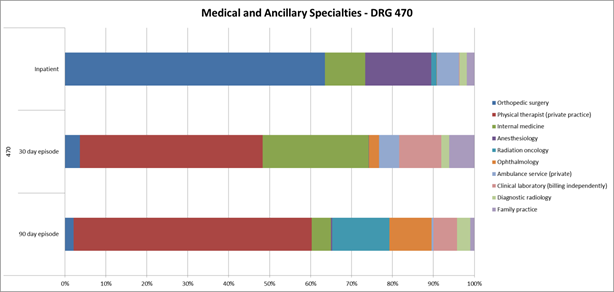
As can be seen from the about chart, the post-discharge costs represent a significant portion of the total cost of the episode.
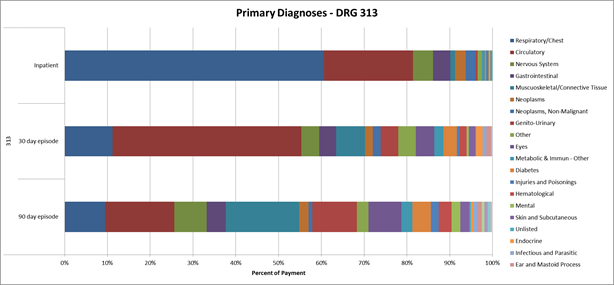
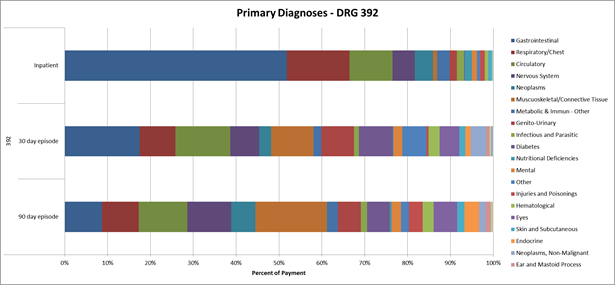
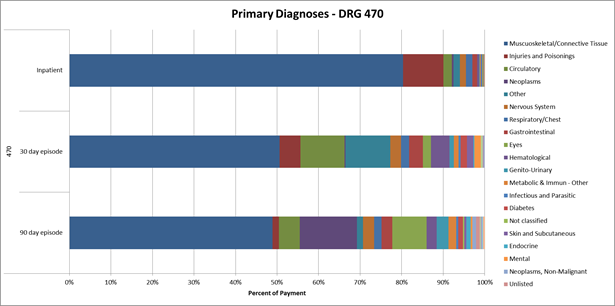
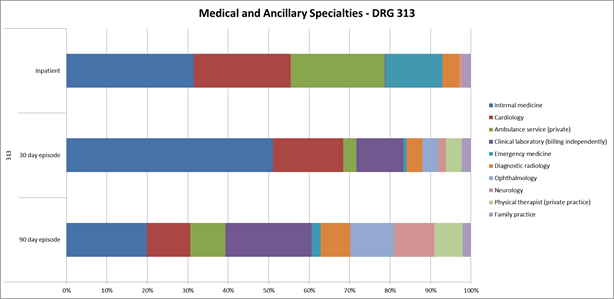
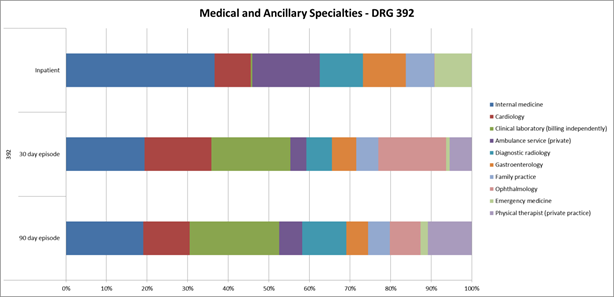
Analysis performed by Singletrack Analytics using the 5 percent sample data Medicare makes available for research demonstrates a significant disparity in diagnoses between those found during the inpatient stay and those found post-discharge. The primary diagnosis on each provider's claim was used, along with the payment amount for that provider's service on that claim. The graphs below show several common Medicare DRGs that may be candidates for bundled payment, with the percentage of payment by diagnosis separated for the inpatient stay, a 30 day post-discharge period, and a 31 to 90 day post-discharge period. DRGs shown are:
- DRG 291 - Heart failure & shock w MCC;
- DRG 313 - Chest pain;
- DRG 392 - Esophagitis, gastroenteritis & misc. digest disorders w/o MCC; and
- DRG 470 - Major joint replacement or reattachment of lower extremity w/o MCC.
Variations in diagnoses
In each DRG, the diagnosis related to the DRG category is the most predominant diagnosis for inpatient services, accounting for more than 50 percent of the provider payment; (Note that physician services provided to inpatients may not necessarily be related to that patient's DRG). However, services provided during the post-discharge period are significantly more diverse and are often unrelated to the admitting diagnosis. This is not surprising given the diversity of illnesses present in many Medicare beneficiaries, but it presents a patient management problem and cost risk to the bundled payment contracting organization. 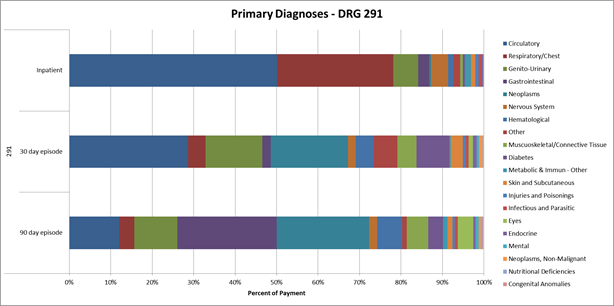
Variations in physician specialties
These variations in patient condition also affect the specialties providing services to these patients. While the network of physicians necessary to provide care to inpatients can be relatively narrow, and structured around the diagnoses of the DRG selected for bundled payment, the physicians who care for patients in the post-discharge period will be much more diverse. The graphs below show the percentage of provider payments to each physician specialty in the above DRGs for the indicated time periods.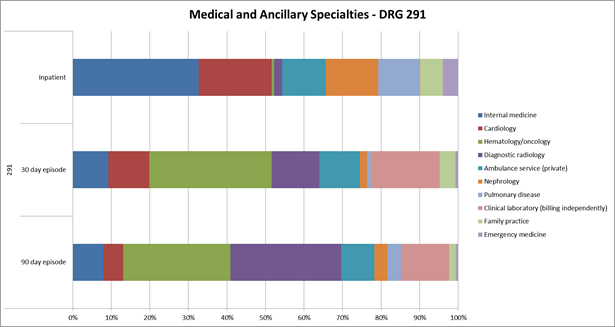
Implications for bundled payment applicants
Several conclusions can be drawn from this analysis. First, it will be critical for bundled payment applicants to carefully examine the data provided to them by CMS to ascertain the distribution of diagnoses and services within their selected DRGs for their patient populations. Treatment patterns vary widely among different populations, and the results shown above may not be indicative of any particular hospital's patient population needs.
Next, applicants should use the results of their analyses for two purposes: first to identify the occurrence of unrelated conditions that may be carved out of a bundled payment for specific DRGs. While CMS is unlikely to allow the omission of conditions that are substantially related to the admitting diagnosis of the patient, they have indicated a willingness to exclude services that are clearly unrelated. But those services must be identified and submitted as part of the bundled payment application or they will be included in the episode.
For services that cannot be carved out of the episode, the applicant must determine how it will deal, if at all, with managing those services. It may be necessary, for example, to incorporate a wider group of specialties within the contacting organization in order to secure their cooperation in managing patient post-discharge care. Given CMS’s interesting care redesign for these patients, it is also advisable that applicants specifically address their plans for post-discharge care follow-up in their application.
While entailing less risk than accountable care organizations, participants in the MBPI will still be financially responsible for a component of care that reaches beyond the walls of hospital. Understanding the extent of these services, and preparing a comprehensive plan to deal with them will be critical to the success under bundled payment.
Learn more about Singletrack Analytics.
More Articles on Bundled Pricing:
Deadline for CMS' Bundled Payment Initiative Approaching
Opportunities in the New Bundled Payment Initiative

