The chief executive officer of a large hospital system recently told me his hospitalist program was too expensive. He didn't believe hospitalists' case loads were sufficient to justify their compensation.
Even though hospitalist programs are a critical part of nearly every U.S. acute-care hospital and one of the fastest growing healthcare specialties, this perception is not uncommon. Finance executives and other administrators look at their hospitalist program as a line-item expense because they analyze the wrong metrics. They know the largest hospitalist program cost is physician compensation and may only measure effectiveness by how many patients hospitalists see in a given day. It's up to hospitalists to change their perception.
Measure the right things
Most hospitalist programs are more valuable than they are given credit. For example, a large Maryland community hospital recently built a new facility that increased its licensed beds by 20 percent and spread the coverage for the hospitalists. The providers' compensation model was based strictly on production. Hospital administrators changed the compensation model to be more quality driven as well as including measures for emergency room physicians and hospitalists to improve their relationships. Team members became leaders in governing the hospital and were indispensable. Quality improved, lengths of stay decreased by 25 percent and average daily patients increased.
Measures such as lower readmissions and shorter lengths of stays along with case mix changes and higher patient satisfaction scores will give them a more complete financial as well as quality picture. The solution is as easy as creating a simple dashboard that includes more extensive metrics, and here's how.
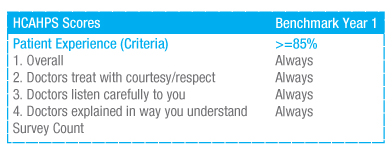 |
| Example dashboard for HCAHPS measure |
Add unique measures such as how quickly the hospitalist sees a patient after the emergency department calls. When the patient is discharged is also important. If they are ready to discharge at 10 a.m. rather than 8 p.m., they are using space more wisely. Hospitalists can also compare industry benchmarks and report on coding distribution.
Document monthly statistics over 12 months to capture the seasonality in hospitalists’ work that sometimes mirrors the same hospital trends.
Drop this data into a simple Excel spreadsheet with section headings similar to the ones shown. The spreadsheet should be easy to read and include financial categories that are important to finance executives.
Once the needed data is gathered, the dashboard will be more meaningful if hospitalists collaborate with hospital leaders in creating the report to address leaders' unique requests and the community's needs. This shows they listen and collaborate as partners in the hospital.
Share the facts
Now it's time to share the information. Many physicians struggle to find the time, right channel and opportunity to communicate to their organization. In fact, 65 percent of medical schools now teach courses on patient communication, and hospitalists can spread these skills to other parts of their jobs to improve the value of their program and ultimately improve the patient experience. Well-run hospitalist programs have regular meetings, at least monthly, with hospital leadership — a prime opportunity to review the dashboard and boost perception of the hospitalist program. Regular staff meetings that include medical directors, ED staff and hospitalists will give peers the opportunity to discuss and align goals, metrics and how each can help the other succeed.
Peer communications are critical
Hospitalists' communications with peer physicians, case managers and their patients is also critical. A Texas metropolitan hospital added advanced practice clinicians and worked diligently with case management. The hospital lowered its lengths of stay and increased its average daily patient encounters by 10 percent. As a result, perception of the hospitalist program improved in an area where they competed with two other local groups for patient population.
In this common example, a patient visits the hospital emergency room complaining of shortness of breath that turns out to be chronic obstructive pulmonary disease. The ED physician decides a patient hospital stay is the best solution, so the hospitalist admits the patient even though they have a different clinical viewpoint. The hospitalist believes the patient should remain in observation status or be treated with medications in the ED. The hospitalist will address it with a peer review later while, in reality, the patient has issues that the ED didn't communicate. This creates a cost rather than quality of care issue for the patient, but more effective communications would lead to a better outcome for the hospital and the patient.
In today's more consumer-driven healthcare market, it's important for hospitalists and case managers to meet with patients and their families so they know when they will be discharged and fully understand their care plan – especially if they will be discharged to a step-down unit. With this example, better communications and daily case reviews would allow hospitalists to start their work with patients more quickly and often discharge patients faster and provide better long-term care. HCAHPS will reflect a more positive experience when patients have information.
In this patient scenario, testing is completed successfully and the patient is discharged, but no one knows if they ever had a follow-up visit with their primary care physician since that physcian never heard about their patient's condition. Hospital staff could take advantage of tablet technology to schedule a follow-up appointment with their primary care physician or refer and schedule an appointment with a pulmonary specialist before the patient walks out of the hospital.
This example shows how clear communications between physicians can decrease the number of readmissions in less than 30 days. If this metric rises, there is a negative financial impact on the hospital as well as possibly causing the patient to be dissatisfied. Conversely, if the patient is admitted but really doesn’t need the additional care and is discharged the next day, patient satisfaction may be favorable, but Centers for Medicare and Medicaid Services would flag the one-day stay for a potential audit.
To help prevent both of these scenarios and provide better long-term care for the patient, ED, hospitalist and primary care physicians must use secure but easy-to-use lines of communication to update all of a patient’s care givers. Here's how one hospital did it. A New Mexico hospital enhanced communications between emergency departments and referring physicians. This community hospital decreased the number of patients leaving the emergency room without being treated by more than seven per day. They also increased admissions by nearly one per day and decreased lengths of stay from more than six to just over three. Daily patient encounters increased from 12 to more than 40 per day with readmission rates dropping dramatically. Core measures reached nearly 100 percent in all categories.
As population health and risk-based care become the norm, HCAHPS will reflect a more positive experience when patients have information. Open communication between hospitalists and hospital administration, emergency room personnel, nurses and case managers will improve the real and perceived value of hospitalist programs giving these important programs the respect they deserve.

